News and Notes from The Johnson Center
Halloween Open House
JCCHD | Mon, October 29, 2018 |
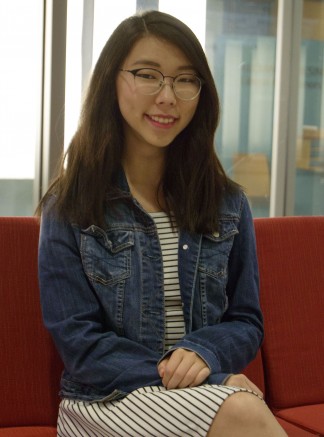
Fall 2018 Interns
JCCHD | Thu, October 25, 2018 |Introducing the Fall 2018 Class of Interns at The Johnson Center!
Here at The Johnson Center, we have a long-standing internship program that is a key part of our day-to-day work. We have hosted college students from across the country who have diverse professional interests; we have had students who were studying to become doctors, nurses, teachers, psychologists, counselors, dietitians, child life specialists, non-profit administrators, occupational therapists, speech therapists, research scientists, and much more. Over 165 students have committed their time, talent, and passion to learn about and improve the services that we offer to our community. In turn, they gain insight and perspective on those we serve and learn all about the challenges and rewards that come from working in such a diverse, complex, and engaging community.
Internships at The Johnson Center are a hands-on experience; interns have been involved in research studies, community events, development of clinical and community programs, assisted in clinical care, and much more.
It is such an honor to have these bright and motivated students join our team and give their time and resources to serve our programs and our community.
Lina Kim is a senior at the University of Texas at Austin, where she is pursuing a BS in Human Development and Family Sciences. Her goal is to attend medical school and pursue psychiatry because she believes that mental health is an area that is not emphasized enough in healthcare due to stigma; she hopes to play a role in changing this. She has been actively involved with the National Alliance on Mental Illness on Campus at UT Austin since its inception and she is a regular volunteer at Dell Children’s Medical Center and Austin State Hospital. Lina is excited about her internship at The Johnson Center and is enjoying learning about the intricacies of this community. She is grateful to be playing a part in supporting people with developmental disorders and their families.
Sherley Ly is a senior at The University of Texas at Austin, where she is studying Human Development and Family Sciences with a concentration in Early Childhood. After graduation, she plans to take a gap year before applying to nursing school. During that year she plans to continue volunteering within the community to gain further insight and experiences in fields related to infants and toddlers. In her free time, she can be caught obsessing over her Corgi-Chihuahua dog, reading a good book accompanied by a cup of coffee, spending time outdoors, or all the above. As an intern, she is excited about her time with The Johnson Center family and she is assisting with the mission of providing educational and positive support and services to ensure that children have the skills necessary to reach their full potential.
Alondra Morales was born and raised in San Antonio, Texas. She is a senior at The University of Texas at Austin, where she is double majoring in Human Development and Family Sciences and Health and Society. In addition, she is pursuing a certificate through the Bridging Disciplines Program with a concentration in Children and Society. Alondra holds a work-study position at the UT Child Development Center as a child-care student assistant. She is interested in attending nursing school after she graduates, with an additional interest in Child Life. Her hobbies include working out, hiking, and playing volleyball.

Erica Santos is a currently a Junior at the University of Texas at Austin, where she is pursuing a Bachelor’s of Science and Arts in Biology and a certificate in Social Inequality, Health and Policy. After graduation, she hopes to attend medical school. As a Clinical Intern at The Johnson Center, Erica shadows clinicians as well as assists with developing resources that help the children and families being served. She is enjoying learning more about multi-disciplinary care during her internship with The Johnson Center and being apart of such a collaborative program.

Madison Tuazon is a 5th year at The University of Texas at Austin, where she is majoring in Biochemistry and Finance and completing an interdisciplinary certificate about children and health. Her goal in the future is to attend medical school and become a pediatrician. Madison is excited to be learning about the clinical assessment and treatment of individuals in the developmental disorder community. She is also excited to be gaining insight into the necessary practices to serve children with developmental disorders and the additional services put in place to assist families. Her internship projects include planning educational outreach programs and inclusive social events for the community.
New Research on the Use of Specific Carbohydrate Diet (SCD) in a Child with ASD, FXS, & GI Issues
JCCHD | Mon, August 13, 2018 | [Autism Treatment][Healthcare][News][Research]New research from The Johnson Center for Child Health & Development was recently published in the Journal of Autism and Developmental Disorders examining the implementation of a Specific Carbohydrate Diet (SCD) for the management of gastrointestinal issues in a child with Autism Spectrum Disorder (ASD) and Fragile X Syndrome (FXS).
This brief report describes data that was collected from a four-year-old boy recruited as part of a larger dietary intervention study. During initial enrollment in the larger study, it was not disclosed that the child had any diagnosed genetic conditions that would exclude him from participating in the larger study and the child was enrolled. Six months into the study, records were submitted that indicated that the child had undergone a genetic evaluation at the age of three that resulted in a FXS diagnosis. This meant the participant did not meet criteria for the larger study and was subsequently removed; data from this participant was subsequently analyzed and published in this case report. Data collected at enrollment and again after 4 months of dietary intervention included anthropometrics, dietary intake, blood markers, gastrointestinal (GI) symptoms, sleep issues, and behavioral concerns.
During the study, all food and drinks that the participant consumed over the 16 week study period was selected and monitored by a dietician to ensure it met the guidelines of the SCD protocol and was prepared by a private chef using local and organic food sources. The child did not consume any food or drinks outside of the prescribed foods provided as part of this study. Weekly counseling was provided to ensure the child had adequate nutrition intake.
After 16 weeks, results indicated that the SCD protocol was well tolerated by the child and led to improvements in growth status and gastrointestinal symptoms, as well as a reduction in maladaptive behaviors such as sensory, repetitive, and ritualistic behaviors, semantic/pragmatic problems, specific fears. Results also documented an increase in adaptive behaviors such as receptive and expressive language, learning, and memory.
Based on these results, more research is needed to further evaluate the use of the SCD protocol in young children with ASD and FXS and GI Concerns.
Citation
Barnhill, K., Devlin, M., Moreno, H.T. et al. J Autism Dev Disord (2018). https://doi.org/10.1007/s10803-018-3704-9
Free Workshop for Parents and Caregivers
JCCHD | Wed, July 11, 2018 | [Applied Behavior Analysis][Autism Treatment][Community][Events][News]You may hear the terms tantrum and meltdown used synonymously, but did you know that they mean different things? Join us for a free workshop for parents and caregivers and learn the differences, as well as strategies to effectively handle both.
This workshop will be presented by Amanda Tami, LPC, BCBA and there will be a small group discussion following the presentation to answer questions and provide additional resources and information.
Free childcare and children’s activities will be available on site for a limited number of participants. Children ages 2-12 will have the opportunity to participate in games, crafts, and activities under the supervision and guidance of staff and interns from The Johnson Center. (To sign up for the children’s activities, select a child’s ticket for each child who will be in attendance).
For more information or to sign up, visit
https://www.eventbrite.com/e/tantrums-meltdowns-outbursts-oh-my-a-workshop-for-parents-caregivers-tickets-42998422439?aff=efbeventtix
_thumb.png)
Counseling for Special Education Professionals
JCCHD | Wed, July 11, 2018 | [Autism Treatment][Community][Healthcare][News]Special educators and related school professionals play a special and important role in the lives of their students. All committed educators and paraprofessionals care deeply and invest an incredible amount of time and resources into the support and education of their students. Special educators often have to go an extra mile or two, coordinating the teaching team that may include the general education teacher, paraprofessionals, behavior specialists, speech and occupational therapists, and more. They may have increased communication with families and must meet an often-staggering level of additional requirements.
It is no wonder that there is a critical shortage of special education teachers and paraprofessionals. In a recent report, 47 states reported shortages of these professionals. Though this challenge isn’t new, it is especially important given that the number of students receiving special education services has been increasing.
Though there are many schools of thought and programs on how best to train, retain, and support special education professionals, many of these plans are missing one critical component: counseling support. Special educators take on an immense emotional burden with each new school year; they must teach to a classroom or body of students with unique and differing needs and may carry these significant emotional challenges home with them at the end of every day.
Special education professionals often report they feel isolated and a lack of shared ownership for the progress and success of their students. They also express concern about the ambiguity of their teaching roles and having less direct instructional time; they are often teaching with general education teachers, co-teachers, specialists and consultants; at the end of the day, who is responsible for making sure the programs are implemented correctly, data is collected, goals are being met, and the child is appropriately and meaningfully taken care of?
Special educators deserve the support and guidance to not only get appropriate training and tools, but to also get the emotional support they need to effectively do their jobs well. This is the reason The Johnson Center for Child Health & Development has created a Special Educator Counseling Program tailored specifically to the needs of Special Education Teachers, Paraprofessionals, and related specialists (Speech, Behavioral, and Occupational Therapists).
These education and therapy professionals often need a sounding board and safe space to discuss their professional and emotional needs and concerns and to learn how to create an effective strategy for handling the stress of their position. Counseling can also include the development of interpersonal and communication strategies that can assist in parent/teacher relationships and relationships between the teacher or specialist and school leadership.
This counselor and teacher/specialist collaboration can be a meaningful and valuable relationship that can prevent burnout, improve job satisfaction, and build new skills to improve professional development and student success.
At The Johnson Center, we firmly believe in the value of counseling services for special education professionals and we are proud to offer services from clinicians who are experienced and dedicated to serving the needs of our community. It is our goal to ensure that appropriate support is available to anyone in need, regardless of financial circumstances. Assistance seeking insurance reimbursement, grants, and a sliding fee scale are available for anyone in need of support.

For more information about The Johnson Center’s psychotherapy services for educators and special education professionals, contact us at .(JavaScript must be enabled to view this email address) or at 512.732.8400.
July Free Webinar: ASD & Depression
JCCHD | Mon, July 02, 2018 |
Do Siblings Need Support?
JCCHD | Mon, July 02, 2018 | [Autism Treatment][Community][Sibling Spotlight]Given the challenges and demands that are often placed on the parents of children with developmental disorders, chronic illnesses, or other significant cognitive or health issues, the needs of the siblings of these children can sometimes be overlooked or underestimated. This makes sense given the more pronounced or immediate needs of their brother or sister.
Siblings of children who have more challenging needs are often dealing with complex feelings and challenges, including:
Loneliness: Siblings may feel that their friends can’t understand what they are going through.
Resentment or Jealousy: Siblings may feel like their sibling’s needs are taken more seriously than their own, or they may resent the time and resources that are dedicated to meeting those needs.
Anxiety or Fear: Siblings may be concerned about their own well-being, the well-being of their sibling, or even be looking ahead and are concerned about what the future holds for their sibling and their family.
Guilt: Siblings may be feeling guilt about not facing the same challenges as their sibling or over adding any demands or concerns to their parents.
Embarrassment: Siblings may be embarrassed by their sibling’s needs or behavior or by the way their family life is affected by these needs.
Frustration: Siblings may be frustrated by their inability to help their brother or sister or by the sibling’s inability to relate to or play with them at the same level. Some siblings also report frustration that they don’t have a “normal” family or can’t do “normal” family things.
Some siblings can become skilled at hiding their fears and feelings, not wishing to place any additional worry or concern on their parents.
At the Johnson Center for Child Health & Development, we have always been committed to supporting the entire family, including siblings. For the past several years, we have hosted a number of SibCamps, designed to offer a fun and supportive therapeutic camp to siblings ranging in age from 7 to 17. These camps have made a positive and lasting impact not only on the children who attend, but also on the entire family. Attendees and their parents have reported that the lessons learned at camp have led to improved understanding and communication between all of the family members.
The success and demand for these camps has revealed a much greater need in our community—counseling services for siblings of children with special needs, provided by therapists with knowledge and expertise on their unique needs.
With the right support and resources in place, supporting the emotional health of every member of the family can lead to more open communication, improved relationships, resiliency, and an ability to see the benefits and unique experiences that can come from being a supportive and supported sibling.
The Johnson Center for Child Health and Development is proud to offer psychotherapy services to siblings of all ages. A sliding fee scale is available as well as a limited number of grants and scholarships. For more information, contact us at .(JavaScript must be enabled to view this email address) or by calling 512.732.8400.

Caring for the Caregiver: Psychotherapy for Parents and Caregivers of People with Special Needs
JCCHD | Mon, June 25, 2018 | [Autism Treatment][Community][Healthcare][News]Parents and caregivers of people with special needs often find themselves facing challenges that would never cross the minds of many parents with typically developing children. From the everyday need to advocate for their child’s best interests to the fear of what the future might bring, special needs parents often find themselves struggling to find a healthy balance. The parents and caregivers of children and young adults with chronic conditions, life-threatening illnesses, and developmental disorders may live in a traumatic state every day as they watch their child experience the challenges that come with their conditions. Living in this constant state of stress is hard on the body and mind, but psychotherapy can help.
What unique challenges do special needs parents and caregivers face?
Burnout – Caregiver burnout is real. Some parents of typically developing children might ask, “How can a parent get caregiver burnout? Taking care of your child is your job.” But caring for a child with special needs is so much more than that. It’s a 24/7 job with little respite, and that’s often on top of your other everyday obligations. When your child has major cognitive challenges or complex medical issues, there is no escape from caregiving. Signs of caregiver burnout are a combination of any of these experiences: feeling constantly run down, feeling like all of the responsibility falls on your shoulders, feeling like you’re consistently on an emotional roller coaster, having no hobbies for yourself, feeling unable to take care of or time for yourself, avoiding social plans, feeling unable to trust anyone else with your child, and getting little rest because your child is always on your mind.
Advocacy – Parents of kids with differences report feeling defensive and ready to put up a fight as default, because they have to spend so much of their lives pushing and fighting to get their child what he/she needs. This world designed by and for neurotypical people often does not understand the needs and challenges of someone with differences, and limited funding, legal power, and knowledge can result in parents having to fight to make everything accessible to their child. This constant battle affects many parents in ways they might not even realize. For example, although a mom thinks an IEP meeting went as well as expected, she finds herself becoming angry when telling a third party about it. The anger fuels her to fight for her child, but it also puts a large, continuous amount of stress on her that doesn’t go away when one fight ends. She knows another one is just around the corner.
Living in danger or pain – When you have a child with special needs, you might feel as if danger is constantly lurking over your shoulders and have to be always on guard. Another seizure or a major meltdown could start at any moment, and some parents live in fear of the pain their children, and in turn they, will experience. Believe it or not, some caregivers of kids with special needs show symptoms similar to those of and are at risk for developing post-traumatic stress disorder; however, for these caregivers, the stressful event, or trauma, is ongoing. How does a person heal when danger or pain remains present? Their sense of safety is non-existent and may need to be rebuilt from the ground up with help from a professional.
Grief – When they find out they are expecting a child, every parent has hopes and dreams of what that child will be. When a child is diagnosed with a life-altering condition, those hopes and dreams change, and that results in a sense of loss for many parents. Even as parents come to accept the diagnosis and what it means for their child, many parents report needing to grieve as their child hits various life milestones.
While life’s challenges will continue and will often be out of our control, psychotherapy can be a brief respite, a first step to increased self-care, a path from pain to resiliency and meaning, and a safe place to experience all of the overwhelming and sometimes guilt-inducing emotions that go with being a parent or caregiver of a person with special needs.
At The Johnson Center for Child Health & Development, we firmly believe in the value of counseling services for parents and caregivers and we are proud to offer services from clinicians who are experienced and dedicated to serving the needs of our community. It is our goal to ensure that appropriate intervention and support is available to anyone in need, regardless of financial circumstances. Assistance seeking insurance reimbursement, grants, and a sliding fee scale are available for people in need of support.
For more information about The Johnson Center’s psychotherapy services and other resources for parents and caregivers, contact The Johnson Center at .(JavaScript must be enabled to view this email address) or 512-732-8400.
Summer 2018 Interns
JCCHD | Wed, June 20, 2018 | [Community][Staff Spotlight]Here at The Johnson Center, we have a long-standing internship program that is a key part of our day-to-day work. We have hosted college students from across the country who have diverse professional interests; we have had students who were studying to become doctors, nurses, teachers, psychologists, counselors, dietitians, child life specialists, non-profit administrators, occupational therapists, speech therapists, research scientists, and much more. Over 160 students have committed their time, talent, and passion to learn about and improve the services that we offer to our community. In turn, they gain insight and perspective on those we serve and learn all about the challenges and rewards that come from working in such a diverse, complex, and engaging community.
Internships at The Johnson Center are a hands-on experience; interns have been involved in research studies, community events, development of clinical and community programs, assisted in clinical care, and much more.
Our Summer 2018 Intern Class is already hard at work on several important projects, including the development of new resource and social programs, translating resources for Spanish-speaking families, coordinating programs that continue to identify unmet needs in our community as well as provide volunteer opportunities, and much more.
Meet the Summer 2018 Johnson Center Intern Class:
Sreeja Atherkode is from India and has a bachelor’s degree with a teaching certification in biology. She worked as a science teacher in India and Dubai before moving to the US. She has a Masters in Special Education (Mild /Moderate Disabilities & Diversities Program) and completed the coursework toward BCBA certification from UT Austin. Her keen interest in the autism field developed due to personal and professional experiences and has entrenched itself and distilled to clinical practice and the research of autism in depth. She hopes that gaining expertise in this crucial field will help her make a difference in the lives of countless children. Today, as humans stand at the cusp of breakthrough research in various therapeutic techniques in different fields, she is excited to be a part of the journey.
Jordyn Jensen is a rising junior at the University of Texas at Austin, where she is studying Special Populations and American Sign Language. She ultimately plans to become an Occupational Therapist. She has previously worked with children with special needs in a variety of settings and she chose to be a summer intern at The Johnson Center because she was seeking to gain experience in a non-profit clinic setting. Jordyn is excited for the opportunity to plan children’s activities for summer workshops at The Johnson Center and she is eager to participate in other programs that will help individuals with autism and their families.

Prageet Kaang is a dentist from India, who is currently pursuing a Ph.D. in Nutritional Sciences at University of Texas at Austin. She has a Master’s in Public Health from Texas A&M University. Her research interests include nutrition and autism, oral health, food assistance programs, diet quality in low-income populations, trace elements, obesity, diabetes and cancer. She has previously worked as a dental lecturer, and currently teaches some undergraduate classes at UT. She is very passionate about community research, especially research involving children and women. In her free time, she likes to volunteer, read books, and watch documentaries.
Kyler Moore is a rising senior at the University of Texas at Austin where she is pursuing a Bachelor’s of Science and Arts in Biochemistry and a BDP certificate in Social Inequality, Health and Policy. Her future plan is to attend medical school to become a physician. Her summer internship priorities are focused on The Johnson Center’s outreach program, Home Cooked Friday’s. With her work in that program, Kyler is getting the opportunity to explore her interests in socioeconomic disparities and public health while gaining experience serving the local community.

Obie Okafor is from Houston, Texas and she is currently a rising senior at the University of Texas at Austin, where she is pursuing a major in Biology with a minor in African & African Diaspora Studies, as well as a certificate in Social Inequality, Health and Policy. Her goal in the near future is to go to medical school and become a doctor, more importantly one that treats and advocates for individuals from under-served communities. As a summer intern at The Johnson Center, she is working on a number of projects, including spearheading an effort to gather recipes and create a Cook Book that will be uses as a fundraiser. Obie says she feels lucky for the opportunity to be an intern at The Johnson Center and is enjoying learning about the way non-profits work and is grateful for the chance to do her part to help communities that are often overlooked.
Maria Pena is a rising senior at the University of Texas at Austin, where she is a psychology major. Her professional goal is to become a clinical psychologist and diagnose and treat children with ADHD, Autism and other neurodevelopmental disorders. Her life goal is to raise awareness of the lack of proper treatment and care currently available for children with special needs in the Dominican Republic, her home country. Maria chose to be an intern at The Johnson Center because she believes this organization is the perfect example of what is needed in less developed countries like her own. She is learning more about the process of understanding children on the autism spectrum and how best to develop personalized care plans depending on their individual needs. Maria says she is glad to get the chance to see first hand how this organization helps people with autism and related disorders and their families with the emotional and financial challenges of supporting a child who has special needs. Her internship projects include shadowing the clinicians and developing materials that she hopes will help people with autism and their families.

Antony Velasquez is a senior biology major at the University of Texas at Austin. His internship projects include working on the Friday community outreach program, including project planning and working with volunteers. When he’s not working at his internship, he works as an EMT for the Georgetown/Austin area and volunteers at a bike shop. His hobbies include political debate, restoring classic cars, biking, and reading.

If you are interested in internship opportunities with The Johnson Center, please email .(JavaScript must be enabled to view this email address) or call 512.732.8400.
Psychotherapy for People on the Autism Spectrum
JCCHD | Mon, June 18, 2018 | [Autism Treatment][Community]Psychotherapy can address some of the skill delays, secondary symptoms, and comorbid conditions that are often associated with autism spectrum disorders (ASD); however, therapy approaches that are successful for people with ASD might be different than those used for the general population, and a skilled and experienced therapist must take this into account.
Here are some areas in which psychotherapy might benefit someone with ASD and things to consider when looking for a therapist.
Who might benefit?
Many people believe that individuals with ASD cannot receive psychotherapy due to cognitive and/or language challenges, or they believe that only people with “high functioning” autism can benefit. While it is true that people with autism who have high levels of insight and need low levels of support in most areas often make the most noticeable progress in psychotherapy, it is also true that even those people with more significant challenges can learn new coping skills with enough self-awareness. An individual who is nonverbal but has another way of communicating can experience interventions and learn new skills just as well as a verbal individual. Someone with low insight but who is aware of their internal and external experiences can learn to share those experiences and gain support.
What challenges might psychotherapy help?
• Anxiety – Providers in the field of autism are increasingly recognizing the link between anxiety and autism, and psychotherapy can provide a safe place to process the world, express feelings, and learn coping strategies. You can learn more about anxiety and autism in The Johnson Center’s webinar available on YouTube: https://www.youtube.com/watch?v=om8Qj6uJmzU.
• Alexithymia – This term refers to the inability to recognize emotions in the self or others, a trait commonly associated with autism. Just because someone does not recognize the emotion, however, does not mean they do not experience it. Someone with alexithymia can struggle to manage their responses to stress, for example, because they don’t recognize feeling angry or scared but still act on that feeling. It can also make forming connections with other people more difficult. If we can’t connect with someone emotionally, we can’t empathize with them or relate to their inner experience.
• Trauma – Most people think of trauma as severe child abuse, a soldier’s experience at war, or a horrific accident. While those things are certainly traumatic, we can’t underestimate the potential trauma of adverse social experiences or overwhelming sensory stimuli.
• Social skills – Psychotherapy is a safe place where an individual can process social experiences; gain perspective on challenges; learn skills to take others’ perspectives, empathize, and follow social expectations; and practice relational skills within a supportive, secure, and safe relationship.
• Emotion regulation – Emotion regulation is the ability to experience an emotion at a level that allows most optimal functioning. Too much emotion or not enough emotion can both be problematic in most scenarios—behaving ”inappropriately” because our emotional intensity doesn’t match others’ expectations. Emotion regulation is a skill that is learned over time, but this can be especially difficult for individuals with autism and ADHD. Psychotherapy can provide skills and strategies needed to experience emotions without becoming overwhelmed by them.
• Obsessive-compulsive and related disorders – Rates of comorbidity between autism spectrum disorders and obsessive compulsive disorders (an entire class of disorders) are high—meaning they often occur together. Although autism can include symptoms like rigidity, rituals, and compulsions, when these get to the point that they interfere with daily functioning, they can be classified as separate disorders and treated as such. Obsessive-compulsive and related disorders are rooted in anxiety, and there are very effective cognitive-behavioral strategies that can help.
Considerations when Looking for a Therapist for a Person on the Spectrum
1. Consider developmental age rather than the chronological age of the person seeking therapy. For example, if a person is 18 but is developmentally in second grade, the therapist needs to use the types of techniques and interventions he/she would use when working with a second grader—bringing in things like play, art, and simpler language but in a way that does not make the person feel as if they are being treated as a child. When choosing a therapist, consider the ages of clients they have experience with and whether or not that matches the developmental age of the client rather than chronological age.
2. Look for a therapist who has significant knowledge about and experience with autism. This does not necessarily mean that the therapist only does psychotherapy with people with autism. Look for someone who truly knows and understands autism, as the clinician needs to be able to identify symptoms associated with autism to effectively treat the client. For example, if a client brings up a topic or a fear repeatedly, a psychotherapist working with a neurotypical client (a person without autism) might conclude that anxiety is present and explore that topic at length. In someone with autism, that topic or fear might be a perseveration—the excessive repetition of an action or speech about one topic. Unlike exploring an intense topic with a neurotypical person, engaging in a perseverative topic with someone with autism can often make it worse. Instead, when a psychotherapist knows how to recognize perseveration, he/she might conclude that there is likely stress, anxiety, or another need for coping behind it and shift the focus to providing calming strategies and support.
3. Deconstruct the “people pleasing” responses. A successful therapeutic relationship is an honest one in which both parties can give feedback and responses that are genuine, without fear that they will be letting the other person down or causing strain on the relationship. In some cases, and even more so for individuals with autism, clients tell the therapist what they think he/she wants to hear rather than sharing their true experience. There are many possible reasons for this, and the therapist needs to be able to identify when this is happening and explore the deeply seeded beliefs, emotions, or skills delays resulting in this response.
4. Think about confidentiality. Unless a caretaker is awarded guardianship, an individual becomes an adult at the age of 18 regardless of their developmental age. Confidentiality is the protection awarded to the relationship between a therapist and an adult client that prevents the therapist from disclosing any information shared with anyone else, except under specific circumstances. You might talk with potential therapists about how they would handle clients with developmental delays who are over the age of 18 but without guardianship in place, as challenges can arise. For example, a parent, caregiver, or other person may need to be present to help with communication between the therapist and client, and some information may need to be shared with the financially responsible party if that party is not the client. Even if the therapist has the client sign a release allowing this sharing of information, how does the therapist know that the client is able to give informed consent? It can be beneficial to talk to the therapist before starting psychotherapy with him/her to iron out details like this and know what to expect regarding confidentiality in this situation.
_thumb.png)
Just like any therapeutic intervention, it is important to access services from experienced, knowledgeable, and dedicated professionals who are committed to understanding the challenges, strengths, and needs that are most relevant to the person seeking assistance and support. At The Johnson Center for Child Health & Development, we take counseling for people on the autism spectrum very seriously and are proud to offer services from clinicians who are dedicated to serving the needs of our community. It is our goal to ensure that appropriate intervention and support is available to anyone in need, regardless of their financial circumstances. Assistance seeking insurance reimbursement, grants, and a sliding fee scale are available for people in need of support.
For more information about psychotherapy for individuals with autism or to learn more about The Johnson Center’s psychotherapy services, contact us at 512-732-8400 or .(JavaScript must be enabled to view this email address).
Take Action for Autism in 2018!
JCCHD | Thu, March 01, 2018 |
Free Webinar 3.1.18
JCCHD | Thu, February 22, 2018 | [Autism Treatment][Community][Webinars]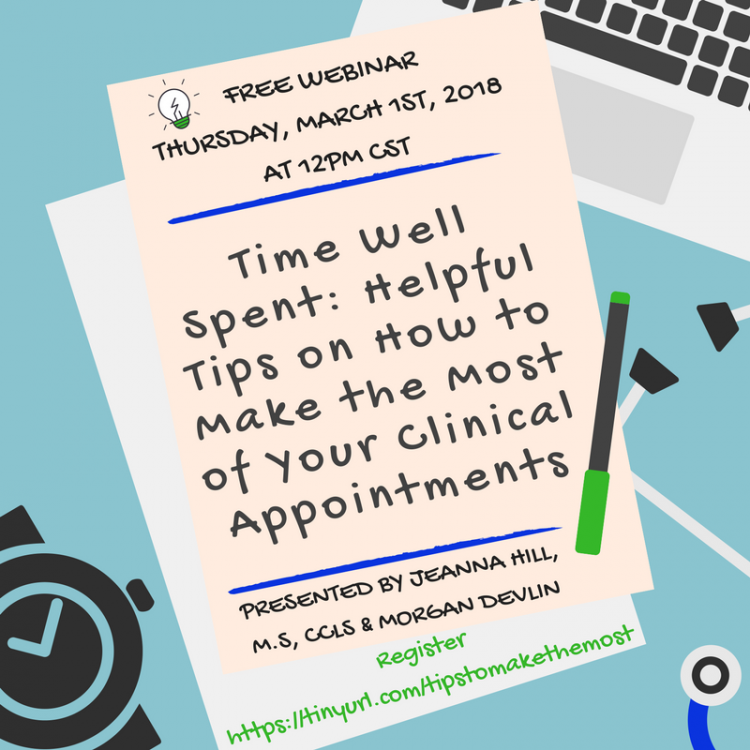
Free Webinar 2.26.18
JCCHD | Wed, February 14, 2018 | [Autism Treatment][Community][Webinars]_thumb.png)
ADHD Workshop
JCCHD | Thu, February 08, 2018 | [Applied Behavior Analysis][Autism Treatment][Community][Events]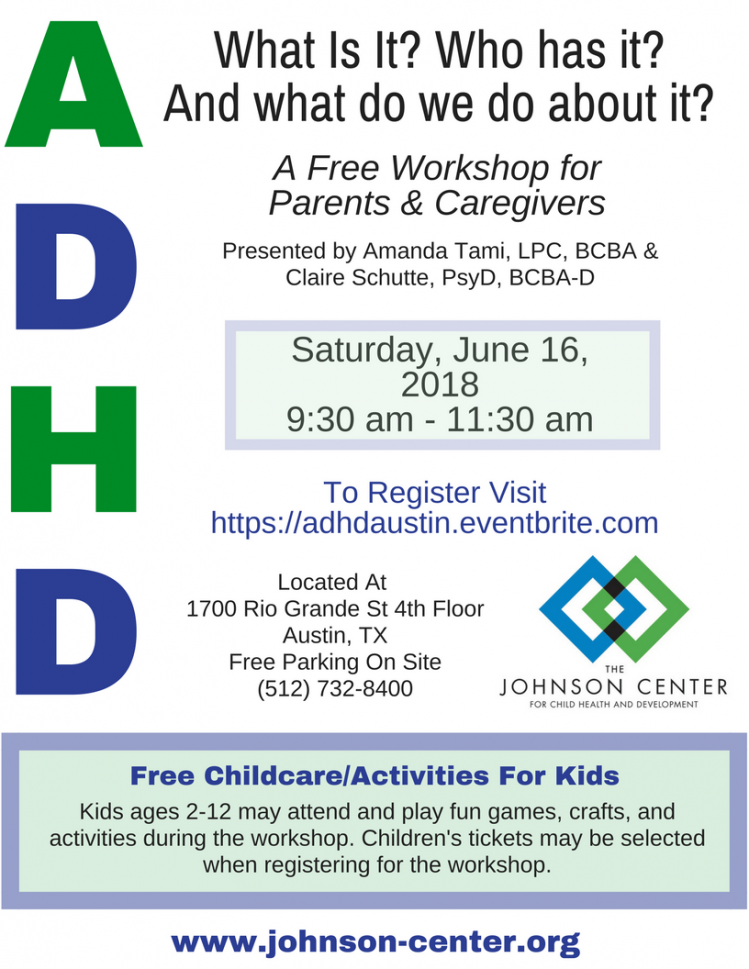
Free Webinar 2.8.18
JCCHD | Wed, February 07, 2018 | [Autism Treatment][Community][Webinars]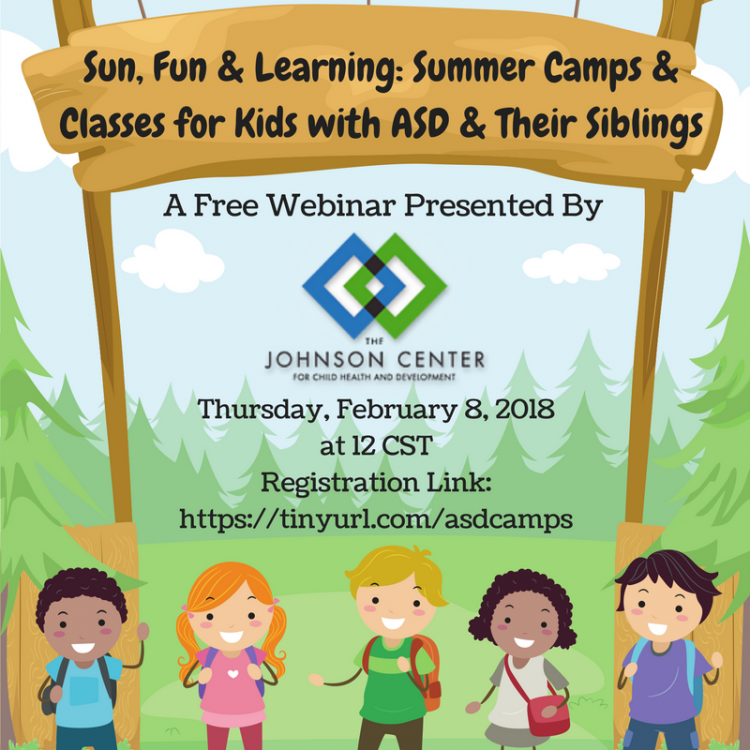
Teddy Bear Clinic
JCCHD | Tue, January 30, 2018 | [Autism Treatment][Community][Events][Healthcare]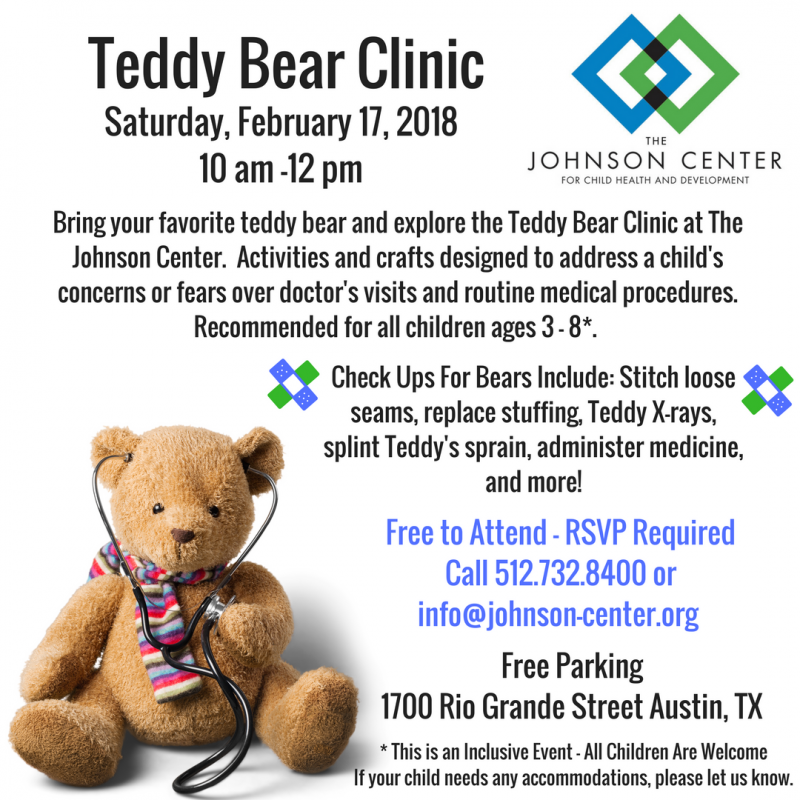
January 11, 2018 Webinar
JCCHD | Wed, January 10, 2018 | [Autism Treatment][Community][Webinars]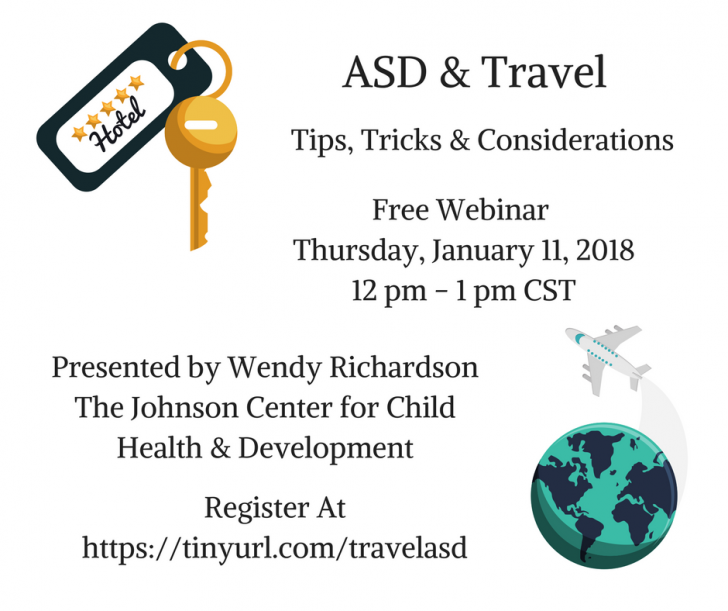
Holiday Open House
JCCHD | Wed, November 15, 2017 | [Community][Events]2_thumb.jpg)
Costumes for a Cause
JCCHD | Wed, November 01, 2017 | [Community][Events]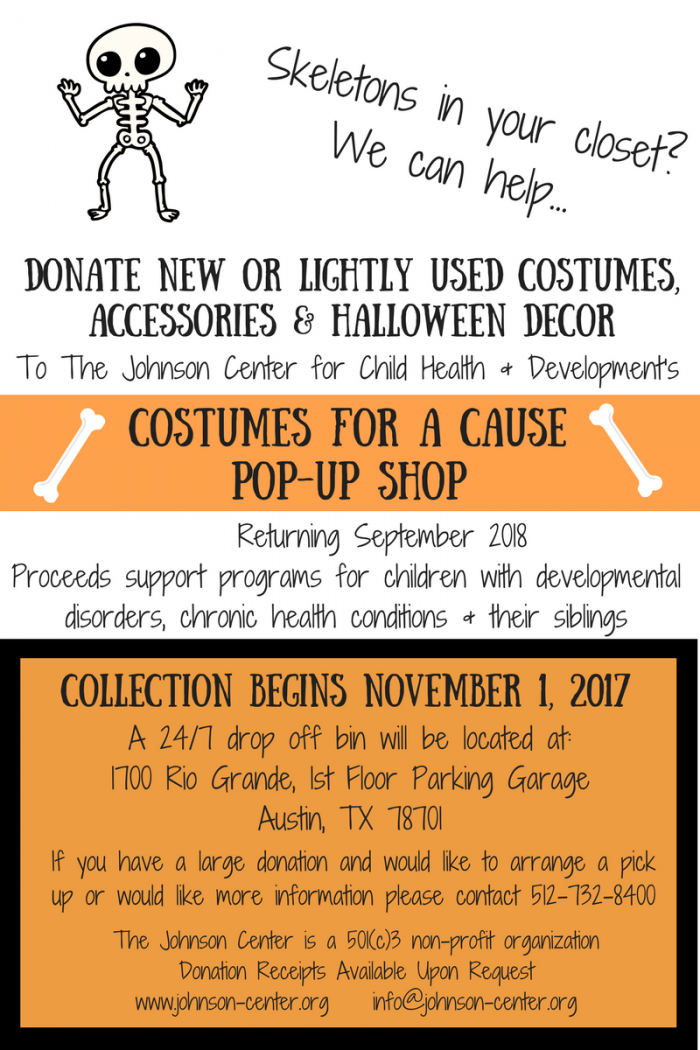
Strategies for Meltdowns
JCCHD | Wed, October 25, 2017 | [Applied Behavior Analysis][Autism Treatment]You may hear the terms tantrum and meltdown used synonymously, but did you know that they mean different things? A meltdown is as an episode that occurs when the nervous system is overwhelmed by social, cognitive, linguistic, emotional, or sensory experiences. The meltdown is a release of tension that typically comes with a big reaction. The person loses control and explodes; this is an involuntary response. They cannot control it—intense emotions take over, and children don’t have the coping skills to manage them. They lose cognitive control and are unable to process and think. When a meltdown happens, recovery is slow, up to 15-20 minutes once the stressor is removed. Adults are not immune to meltdowns, either. They may have learned more strategies to better regulate their nervous systems, but getting overwhelmed happens to everyone at times.
A tantrum, on the other hand, is a deliberate response to frustration. This is a learned behavior, and the child has the cognitive control to choose to do it. Tantrums happen because they have been reinforced—they have worked in the past to get the child something. Tantrums can become emotional blackmail—parents and others give him whatever he wants so that he doesn’t have a tantrum. Recovery from tantrums is instantaneous once the child gets what he/she wanted. The tears immediately stop when you give him the toy, for example. In cases of tantrums, we need to determine the function—what does the child get out of this?
Thinking of meltdowns and tantrums in this way, our response to each will be different. For a meltdown (nervous system overload), it is best to proactively prevent them. When they do happen, solitude and reassurance are the go-to response. Use as few words as possible. During a meltdown, your child’s emotional brain takes over and the rational and processing brain is off. This includes focusing on and understanding language. They can’t comprehend explanations or logic right now, so provide calming tools to help calm their nervous systems so that their processing brains can come back online.
In contrast, remember that tantrums are intentional and deliberate; therefore, you do not want to negotiate or give in—doing so would provide reinforcement and make the tantrum more likely to happen again. Assertively and calmly explain the child’s choices and consequences, and then stick with them. For more information on dealing with tantrums, please see our webinar Tantrums and Meltdowns: Oh My!
If your child has frequent meltdowns, consider speaking with a psychotherapist or counselor about anxiety or emotion regulation issues your child might be having. Remember that a meltdown happens when the nervous system is overwhelmed. A child becomes overly anxious, scared, angry, or even happy and their emotions become intense and overtake rational thought. While adults might have coping strategies to prevent emotions from becoming overwhelming or to manage them if they do, children don’t have these resources yet, so something an adult would see as a small problem might feel really big to a child and lead to this reaction. Below are some tips for helping your child through a meltdown.
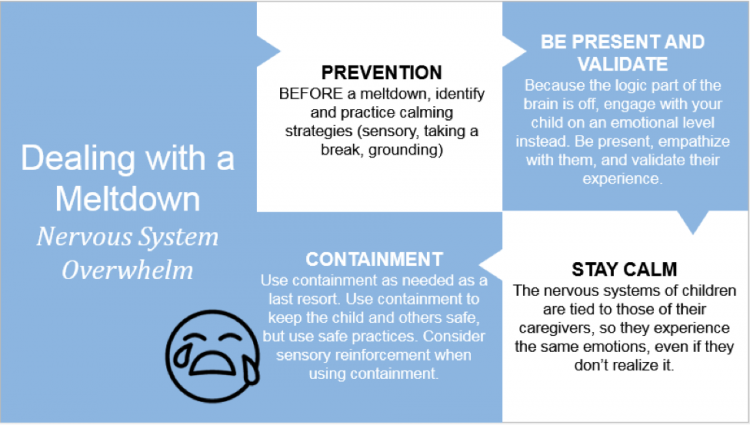
1. Prevention is the best “cure” for a meltdown. Once a child is in the meltdown state, it takes some time for them to come out of it. Preventing them from getting to that point is best. As parents, know your child’s triggers, and teach them to monitor their body in order to be able to identify when they may become overwhelmed. Help them learn how to communicate when they start to feel overwhelmed and need a break. Check in with them in situations that you know cause intense emotions, and encourage calming strategies if you see a meltdown coming on. Calming strategies can include taking breaks from the stressful situation; moving to a calm environment; using grounding techniques like mindfulness activities or wiggling fingers and toes; and using sensory tools like silly putty, a weighted blanket, or a fidget toy. Experiment to find what helps your child to feel calm BEFORE a meltdown ever happens so you know what to turn to when you need it.
2. Be present and validate the child. Sit with them as they are going through this uncomfortable experience and engage with them emotionally. Show them that you feel what they are going through and understand it. DO NOT try to problem solve, fix it, ask questions, or distract them. Name the emotions, tell them it’s okay to feel that way, and let them know it’s normal and this will pass. Some kids might prefer to be left alone during this time, and that’s okay. Just join them in the emotions they are feeling using as few words as possible—no explanations or lecturing.
3. Parents should do their best to stay calm during their child’s meltdown. The nervous systems of children are tied to those of their caregivers. When parents feel scared, the child senses this and feels scared, too. If you get angry or anxious when your child has a meltdown, it will likely make it worse. In addition, Tony Attwood, an Asperger’s expert, says that many people with autism have a sixth sense in which they are able to intuit and feel the negative emotions of others. They can be hypersensitive to others’ anger, sadness, frustration, and disappointment. So if you’re angry, even if you don’t show it, they know it.
4. Use containment techniques as a last resort if necessary to keep your child safe. If the child poses a safety threat to him or herself or others, use safe practices to contain him or her. When using containment, especially if you use it routinely, consider whether it might be giving the child reinforcing sensory stimulation. If this is the case, have other sensory-stimulating activities in the environment to reduce the need for containment.
It is possible for a child to learn that their meltdown got them some form of reinforcement, and then the behaviors may become deliberate. Once you get through the meltdown, go back to whatever tasks the child might have missed because of it so that they don’t learn that a meltdown gets them out of something, and/or have them practice and reinforce appropriate behaviors for getting attention or access to toys or activities so they don’t learn that meltdowns are an effective way to communicate what they want or need.
For more information on dealing with tantrums, please see our webinar Tantrums and Meltdowns: Oh My!
Free Fall-O-Ween Open House
JCCHD | Mon, October 02, 2017 |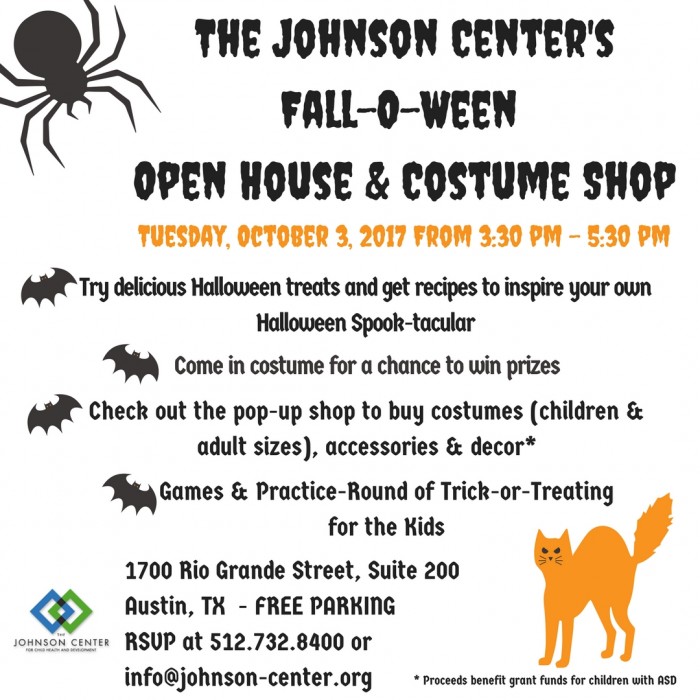
New Research Finds Children With ASD May Be At Risk for Suboptimal Bone Development
JCCHD | Fri, September 08, 2017 | [News][Research]New research published in the Journal of Autism and Developmental Disorders identifies reduced bone mineral density (BMD) in 4-8 year old boys with Autism Spectrum Disorders (ASD) compared with healthy age-matched controls.
In this study, boys diagnosed with ASD had significantly lower spine BMD compared to age-and gender-matched controls, but this was not correlated with any biochemical markers in the blood, dietary intake of calcium or vitamin D (important for healthy bone development), elimination diets, or gastrointestinal (GI) symptoms.
Specifically, boys with ASD who were on a supported (meaning they were under the care of a qualified nutritionist or other healthcare professional) gluten-free, casein-free diet had greater overall intakes of calcium and vitamin D compared with boys with ASD who did not report any dietary restrictions. This provides evidence that dietary intervention in ASD, such as a gluten-free and/or dairy-free diet, which is frequently implemented to address feeding issues, food allergies, or GI concerns, does not result in deficiencies in calcium and vitamin D, or reduced BMD when implemented under the supervision of a qualified clinician.
The study results also indicate that boys with ASD reported significantly greater GI symptoms than boys without ASD, though this was not correlated with BMD status. And contrary to the interpretation of results in prior published studies, this work finds no evidence of reduced BMD in the managed use of a gluten and casein elimination diet, indicating that other factors are involved.
“The data from this study suggests that nutrient intake and dietary status are not contributing factors to the observed decrease in Bone Mineral Density in boys with Autism Spectrum Disorders” explained Kelly Barnhill of The Johnson Center for Child Health and Development, one of the principle investigators working on the study.
Citation
Bone Mineral Density in Boys Diagnosed with Autism Spectrum Disorder: A Case-Control Study. Barnhill, K., Ramirez, L., Gutierrez, A. et al. J Autism Dev Disord (2017).
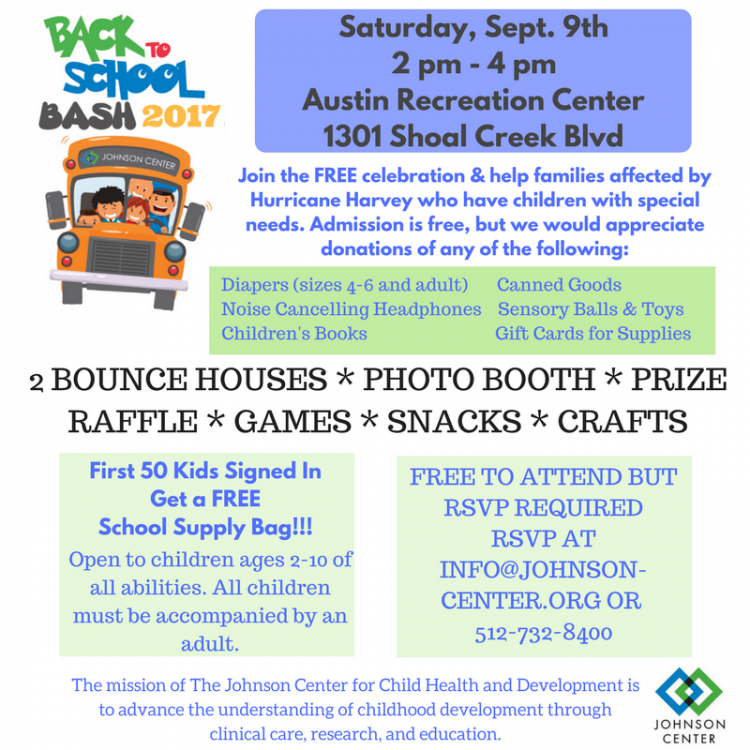
Back to School Bash 2017!
JCCHD | Fri, September 01, 2017 |Come out and enjoy the free family fun and make a donation for children with special needs and their families who have been impacted by the storms. Can’t make it but still want to help? Check out the Wish List by clicking here.
Helping Children Cope With Natural Disasters
JCCHD | Tue, August 29, 2017 |The recent devastation from Hurricane Harvey is a challenge for all who are living through it. For children, a natural disaster can trigger fear and comfort-seeking responses. Older children might look for information, and as they are able to think ahead to what comes next, they might feel helpless. For a child with autism, the chaos surrounding the events can make these feelings can be even bigger. Parents are understandably overwhelmed with the family’s survival and may feel at a loss with how to help their children cope. Here are some tips for helping children during this time of crisis.
- Try to manage your own fears and anxiety. Children are especially keen on the emotions of others, even if they don’t realize it. Their nervous systems are tied to those of their caretakers, so if you are scared, your child feels it and is scared. This is a terrifying situation, so of course you are scared. Do what you can to take care of yourself and manage your own fears, and your child’s will decrease, too.

- Calmly explain to your child what is happening in simple language, validating their emotions, and share with them what steps you are taking to keep the family safe. “The water is coming through the door now. That feels really scary, because you don’t know what is going to happen. I’m scared, too, but I have moved all of the food upstairs and we will stay up there where it is safer.” Even children who are nonverbal benefit from the calm explanation and acknowledgement of feelings.
- Be honest but reassuring. Your child knows something is happening. Denying or downplaying it will decrease their trust in your relationship. Learning more about what is happening can decrease the anxiety that comes with the mind’s what-ifs.
- Keep your child’s normal routine as much as possible. This may be extremely difficult if many of your belongings are destroyed or you’re in a shelter with hundreds or thousands of other people, but try to keep the same meal times, send your child to school if it’s open, and continue your usual bed time routine. Take walks (if it’s safe), play games, and read books in your down time to take your child’s mind off the crisis for a short time.
- Limit media exposure. While parents want to keep on top of the latest information regarding the disaster, young children are unable to put the information they hear through the media into context or know that they may not be in the same danger they see others in.
- Provide opportunities for children to help with planning and making choices about small things that affect them. This increases their sense of control and gives a feeling of empowerment, which is needed in this time of helplessness.
We will share more support resources in the days and weeks to come. If you have any specific questions about caring for the emotional and mental health needs of children affected by the storm, please feel free to reach out to us and we will do our best to provide an answer or a resource that may help you.
Current Resources:
Note: Some of these resources are for all parents and caregivers and some are specific to those with family members who have autism or other disabilities. Special thanks to the Autism Research Institute and Autism Society of Texas for sharing some of these resource links.
- For help identifying and dealing with the stress and trauma of a natural disaster, the National Child Traumatic Stress Network has resources and information here.
- The Disaster Distress Helpline offers crisis counseling and information to people of all ages: 1-800-985-5990.
- For those who have been displaced and are in the Austin area, the YWCA offers free support groups and crisis counseling: 512-326-1222.
- For more information about coping for children and teens about a natural disaster, the University of Minnesota and National Association of School Psychologists offer some useful tips on their websites here and here.
- The Substance Abuse and Mental Health Services Administration provides links to more resources on the topic for parents here.
- The Red Cross is coordinating relief efforts and has disaster recovery information and lists of open shelters on their website here.
- The Federal Emergency Management Agency (FEMA) is providing relief to the state of Texas and to individuals for disaster recovery. You can find information and apply for financial assistance through FEMA on their website here.
- Find information on the Unlocking Autism Grants for families with children with autism here.
- Information on Disaster Safety for People with Disabilities from the Red Cross can be found here.
- Contact the Texas Health & Human Services here.
- Texas 211 provides a voluntary registry for people who need assistance and evacuation in the case of a hurricane or natural disaster. The public may register year-round. Registry information will be forwarded to local Offices of Emergency Management (OEMs). Local OEMs have the responsibility for coordinating evacuations.
- State of Texas Emergency Assistance Registry (STEAR)
STEAR provides citizens with a means to voluntarily register their needs during an emergency response. This registry was developed for people who need assistance during an emergency response, including evacuation assistance during a hurricane response.
- Austin Disaster Relief (aid throughout Texas, not just Austin)
https://www.adrn.org
- Partnership for Inclusive Disaster Strategies - Hotline for Harvey: Phone: (800) 626-4959
Website here.
- Portlight
Hotline for Harvey: (800) 626-4959
Website here.
- Autism Speaks Natural Disaster Resource information can be found here.
AutismSpeaks Cares provides financial support for families affected by autism during natural disasters and other catastrophic life events. The grant program helps families to cover costs associated with critical expenses related to the well-being of the family member with autism on a case-by-case basis. Contact the Autism Response Team. Contact by calling 888-288-4762, or en Español 888-772-9050, or by emailing .(JavaScript must be enabled to view this email address).
- The ARC of Texas Resource Page can be found here.
We will share more support resources in the days and weeks to come. If you have any specific questions about caring for the emotional and mental health needs of children affected by the storm, please feel free to reach out to us and we will do our best to provide an answer or a resource that may help you.
Take Action for Autism in 2017!
JCCHD | Mon, April 03, 2017 |
April is Autism Awareness Month and while awareness is good, the autism community wants and needs action!
What can you do?
~ Check out the Action for Autism Auction and bid on amazing items like tickets to concerts, great dining, shopping, entertainment, and more. The online auction opens April 21st and closes on April 30th. All proceeds from the auction will help provide summer programs and counseling for people with autism and their families.
Check out the great selection of auction items and register to bid by going to
www.charityauction.bid/takeactionforautism
~ Read and sign the pledge to support the autism community in ten meaningful and supportive ways:
Take the Action for Autism Pledge By Clicking Here
Your support and assistance can make a big difference in the autism community!
Amplify ATX!
JCCHD | Thu, March 02, 2017 |It’s that time of year! Click here to Amplify ATX!
1_thumb.png)
Ho Ho Ho - It’s Mr. and Mrs. Claus!
JCCHD | Tue, November 15, 2016 |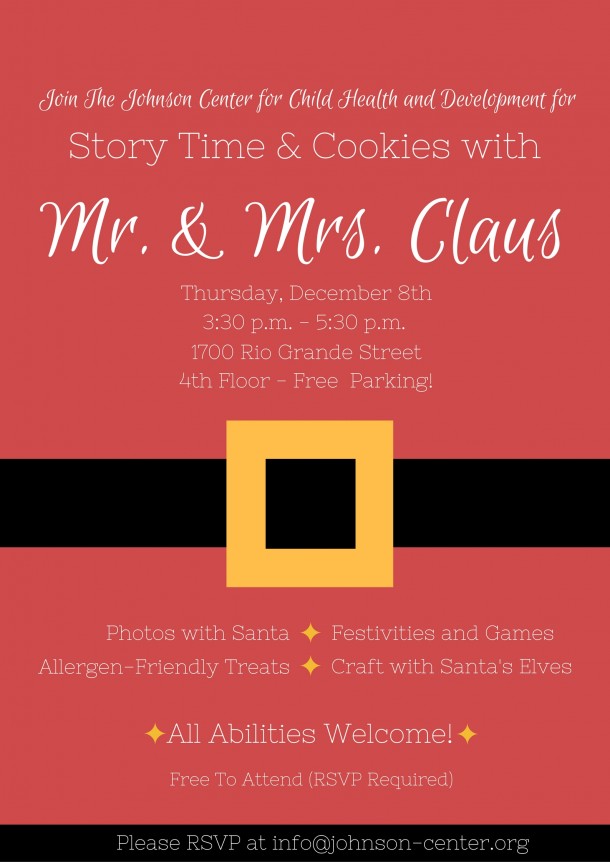
Don’t miss your chance to meet Mr and Mrs Claus in a sensory friendly environment. This free event includes photos with the big man himself, allergen friendly treats, story time with Mrs Claus, and more! Don’t miss out! Email .(JavaScript must be enabled to view this email address) to RSVP today.
Pilot Program Takes Off In January, 2017
JCCHD | Tue, November 15, 2016 |1.jpg)
The Pilot Program at The Johnson Center is a preschool preparatory program for children ages 2-6. The aim of this inclusion program is to increase school readiness and provide families with access to quality behavioral services in a clinic setting at an affordable price.
The upcoming spring session of the Pilot Program consists of 12 hours a week of quality intervention provided by a lead teacher, trained therapists, and supervised by a Board Certified Behavior Analyst. All services occur on-site in order to provide access to age and program-appropriate toys and stimuli, frequent opportunities for supervision and training, and as social opportunities with the other children in the program. Parent training and home goals are also discussed as part of the team meetings.
The program is structured and scheduled in order to maximize a child’s learning opportunities during their time at The Johnson Center. There are designated times for learning new skills, expanding and increasing language, and interacting with peers. Using ABA techniques, the staff members in the Pilot Program teach a variety of skills that may include self-help, gross motor, fine motor, speech, language, listening skills, school readiness, social interactions, and play. All of the goals are individualized to the needs of each class.
The program is implemented by therapists trained at The Johnson Center, and are supervised by Amanda Tami, LPC, BCBA (Board-Certified Behavioral Analyst).
For more information about participating in the Pilot Program, please contact Jeanna Hill, Child Life Specialist at .(JavaScript must be enabled to view this email address) or call 512.732.8400 to schedule an intake appointment.
Donate your Halloween Costumes and Decor
JCCHD | Mon, October 31, 2016 |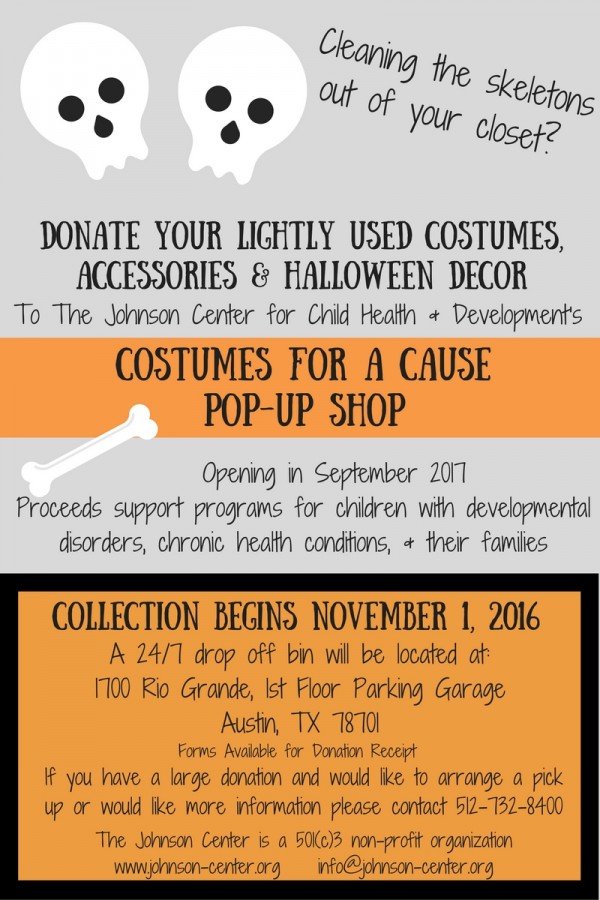
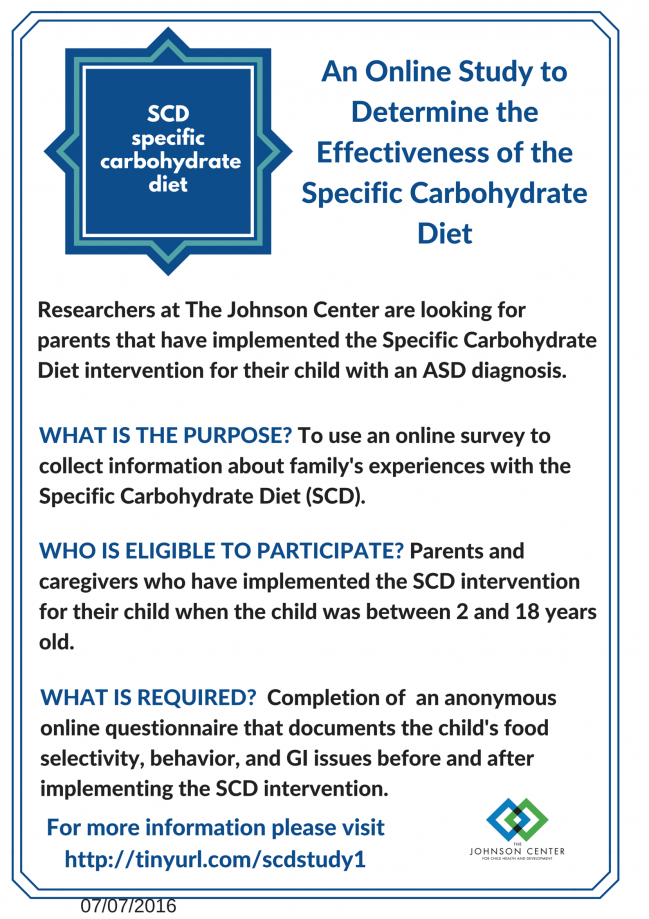
SCD Study
JCCHD | Mon, July 25, 2016 |The Johnson Center for Child Health and Development is undertaking a new questionnaire-based research study to evaluate the effectiveness of the Specific Carbohydrate Diet (SCD) in children with ASD. If you have implemented the SCD for your child when they were between 2 and 18 years of age, we would greatly appreciate your completion of this anonymous, on-line questionnaire. For more details, please click here.
Social Empowerment Group for High School and College Students
JCCHD | Sat, July 02, 2016 |_thumb.jpg)
Free Junior Scientist Event this Saturday
JCCHD | Tue, June 14, 2016 |There is big excitement this week at the Johnson Center – our Junior Scientist event is happening this Saturday! We’ve been planning this event for a while now and we can’t wait to see all of the young scientists in action.
The idea for the Junior Series came from our very own head of research, Dr. Laura Hewitson, who will have her own booth showing participants how to make their own lava lamps. We have worked hard to plan an event where kids could come together and learn about a variety of different sciences – from chemistry to engineering, paleontology to meteorology – while also having fun. Science is all about wonder and exploration, and we have tried to capture that in the booths and activities that are planned.
There will be several great activities for children ages 4-10, including the UT Science Lab booth where kids can make homemade goo, bouncy balls and self-inflating balloons. Kids will be able to dig for fossils and learn about dinosaurs. And our friend from KXAN, Rosie Newberry, is bringing back her interactive tornado to teach us about weather. As an added bonus the first 10 kids who sign up this Saturday will be able to go on a tour of KXAN!
We’d love to have you at our event. Admission is FREE and there will be some activities for younger siblings (under 4) and a place for parents to relax.
WHEN: Saturday, June 18th, from 1PM-3PM
WHERE: Austin Recreation Center, 1301 Shoal Creek Blvd. Austin, TX
RSVP: .(JavaScript must be enabled to view this email address) (All activities are free, but RSVP is required to make sure we have enough supplies and goodies for everyone)
All abilities are welcome. If you or your child needs any special support or accommodations, please let us know with your RSVP and we’ll make every effort to meet your needs.
Sibling Leadership Council
JCCHD | Tue, May 17, 2016 |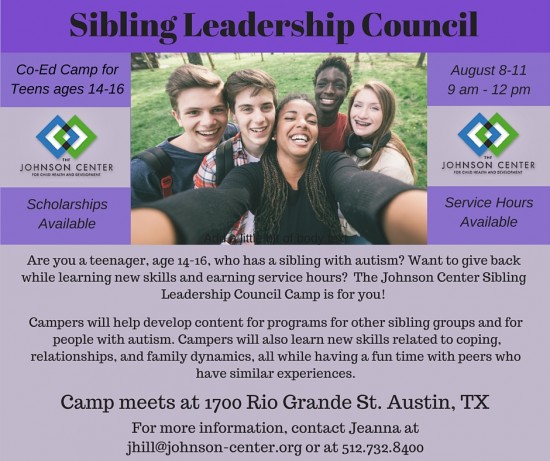
Summer Sibling Camp
JCCHD | Tue, May 17, 2016 |_thumb.png)
Positive Peers Summer Camp
JCCHD | Tue, May 17, 2016 |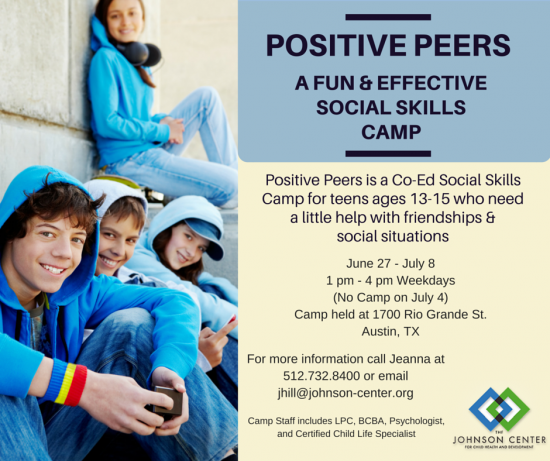
Nutrition & Adolescents: A Time for Change Calls for Changes
JCCHD | Tue, May 17, 2016 |_thumb.jpg)
Friendship Camp for Social Skills Building
JCCHD | Thu, May 05, 2016 |
Take Action for Autism!
JCCHD | Tue, April 19, 2016 |
April is Autism Awareness Month and while awareness is good, the autism community wants and needs you to take action!
What can you do?
~ Check out the Action for Autism Auction and bid on amazing items like tickets to concerts, great dining, shopping, entertainment, and more. The online auction opens April 22nd and closes on April 30th. All proceeds from the auction will help provide summer programs for people with autism and their families.
Check out the catalog of over 145 amazing items and register to bid by clicking here.
~ Read and sign the pledge to support the autism community in ten meaningful and supportive ways:
Take the Action for Autism Pledge By Clicking Here
Your support and assistance can make a big difference in the autism community!
Participate in Autism Research
JCCHD | Sat, April 02, 2016 | [Autism Treatment][Community][Q and A ][Research]April is Autism Awareness Month, but here at The Johnson Center we are calling for an Autism Action Month!
When you live in or work with the autism community, you experience the highs of celebrating the milestones a child reaches and you experience the lows of seeing a child or a family struggle.
One Johnson Center team member recalls an experience that has stayed with her: she once received an envelope with a handful of dollars and a baggie of coins in it. These were funds that a child’s classmates had collected to help him get the feeding therapy he needed. A class of 7th graders in New Jersey donated their weekly allowance for their classmate in need, doing whatever they could to help.
Not everyone has an allowance to donate, but everyone can make a difference. One great need in the autism community is volunteers to participate in research, including people who do not have autism (to serve as controls). One of the biggest challenges our research assistants face is not triple-checking data or perfecting spreadsheets for the statisticians, but finding people to participate in studies. While 90% of children with cancer are enrolled in clinical trials, only 5% of children with autism participate in research.
Here’s the great news - all children can participate. A participant does not need to have an autism diagnosis in the family to do something. Research studies often need typically developing children for comparison purposes, as well as children on the autism spectrum.
For Autism Action Month, check out some of the studies you or your children can enroll in to help the autism community. In addition to the studies at The Johnson Center, you can participate in autism research TODAY, without even leaving your computer:
INTERACTIVE AUTISM NETWORK [IAN) https://www.ianresearch.org/
The innovative online project is designed to accelerate the pace of autism research by allowing parents to report information about their child’s diagnosis, behavior, environment, services received, as well as progress over time. IAN research provides a secure online setting where those affected by autism and their families are active participants in ASD research. By participating in IAN Research, you can help make new discoveries and empower advocates to improve the lives of children and adults with ASD.
AUTISM MATCH https://autismmatch.org
The goal of AutismMatch is to connect families and individuals living with autism with researchers, based on the belief that effective treatments will follow from a better understanding of the causes of ASD. AutismMatch is a community-based registry of people with ASD, their families, and typically developing people who are interested in learning more about autism research. Once enrolled, families will receive periodic contact by email from the Center for Autism.
Quick, Google it. You can support research in other ways.
• Is there autism research happening at a clinic in your hometown? At your local university? Check out some of the studies happening at The Johnson Center right now.
• Find an autism research organization in your town that needs your photocopying prowess, your filing finesse, or help serving snacks at an event bringing awareness to autism research.
• Volunteer to spread the word! If you know of a study that is recruiting, volunteer to spread the word to your friends or family or offer to hang research flyers at community centers, coffee shops, or schools and day
cares in your town.
What if you could join a team of scientists, physicians, patients, and families working together to accelerate progress in autism research? Would you do it for your own child? Would you do it for for your best friend’s child? Would you do it for the other 1 in 68 children who will be diagnosed with autism? Participate in autism research and make a difference in your community.
Inclusion Beyond the Classroom
JCCHD | Sat, April 02, 2016 | [Applied Behavior Analysis][Autism Treatment][Community][Events]Programs for Siblings of People with Autism
JCCHD | Sat, April 02, 2016 | [Autism Treatment][Sibling Spotlight]Growing up with a brother or sister who has autism is a unique experience. Research suggests that siblings often experience difficult emotions including guilt, anger, resentment, loneliness, envy, embarrassment, and anxiety. Siblings may feel as though they get less attention, their needs are not a priority, they are expected to behave perfectly all the time, or they are the only ones who have ever had to live with a sibling with autism. Embarrassment around their peers can occur and some are at risk of being bullied. Adolescent siblings may believe they have increased responsibilities or feel more pressure to succeed.
These emotional challenges can also result in physiological responses. Depending on their age, some siblings may have trouble identifying and expressing these emotions, which in turn can affect sleep, diet, and behavior. Siblings may also develop high anxiety resulting in physical issues or panic attacks. They sometimes express these feelings openly, but many bottle them up inside because they feel ashamed or don’t want to put further stress on their parents. Support strategies that help siblings identify and positively express these emotions can help reduce these risks.

One way siblings can learn support strategies is by participating in sibling support programs. Facilitated discussions and therapeutic play help siblings learn to express their emotions in a supportive environment and connect with others who share similar concerns. These programs also provide lifelong skills that are necessary to build positive relationships with peers, increase self-esteem, and communicate effectively with family members.
The Johnson Center is committed to supporting all family members, including siblings. For several years now we have offered ongoing sibling groups or sibling camps for various age groups. Lead by a team of counselors, psychologists, and child life specialists, our sib groups implement activities that focus on specific learning objectives including: understanding autism, family and peer issues, identifying feelings, and coping and problem solving. Past camps have integrated art, yoga, songwriting, writing, and acting. In our office, we have a growing coping garden from previous sib camps in which participants shared fun coping ideas on each leaf. Previous activities also included creating a Sibling Advice Column in which siblings can offer advice to one another. This activity increases emotional awareness, creates opportunities to connect with peers, and helps to support and validate siblings’ feelings.

By implementing fun and expressive activities we hope to create a toolbox of positive skills siblings can use to help build stronger relationships within their family and community. Siblings learn how to positively communicate their concerns and feelings to their parents and have a stronger bond with their brother or sister. We understand that this is a critical time for all family members, especially young siblings. We hope that by offering support now, we can help shape and build positive family relationships for the future.
Supporting People with Autism in the Workplace
JCCHD | Sat, April 02, 2016 | [Autism Treatment][Community]As the rates of autism have gone up, so have the number of people with autism facing the transition to adulthood and employment. This has presented the need for more vocational opportunities for adults with ASD. Most people with autism would like to work; however, lifetime employment rates are low. Many companies are starting to recognize the great value in hiring employees on the autism spectrum. This includes increased workplace diversity and a sense of inclusion among both employees and customers. In turn, employees with autism can expand their potential, independence, and self-esteem.
Employees with autism have unique skill sets to contribute to the workplace, often including:
Attention to detail: Focus and attention to detail are typically areas of strength leading to efficiency and productivity.
Reliability and adherence to schedule: Many individuals with autism thrive on routine and schedule, often making them reliable team members with a strong work ethic.
Specific talents and passion: Individuals with autism often have special interests and talents that they can bring to the workplace. If a job is a good match to these interests, employees with autism can bring passion, expertise, and innovation.
Unique perspectives: Employees with autism can offer unique and creative perspective contributing to problem solving, creativity, and “out of the box” solutions.
There are many things employers can do to support people with autism in the workplace. It is important for companies to have an understanding of the strengths and challenges associated with autism. This can be learned through educational resources as well as from potential employees themselves. Important things to keep in mind are the type of work environment that provides the best fit, common social and communication difficulties associated with autism and how to navigate these, as well as certain behaviors common to autism. For example, many individuals with autism have sensory sensitivities and may work best in a quiet environment free from sensory distractions. An employee may be better able to communicate their thoughts clearly via email rather than face to face. Many individuals with autism learn well with visually presented information, so the use of pictures, visual schedules, lists, or videos may help them best learn work tasks.
All individuals with autism have some differences and challenges with how they communicate and engage, as well as with their behavior and thinking style. However, it’s important for employers to be aware that all people with autism are unique in their own way, including their interests and skills as well as challenges.
Traditional interviews can be difficult for anyone, particularly individuals with autism. Social behavior such as eye contact, poise, and communicating clearly can be areas of difficulty and hinder their ability to present well. Therefore employers should be aware of this during the interview process and consider giving individuals a trial period to see how they learn and perform the expected tasks.
Vocational rehabilitation programs can work with companies and individuals with special needs to support positive outcomes in the workplace. They offer a variety of support services from educating the workplace personnel to providing on-the-job coaching. Another good idea is to assign a mentor co-worker to help the employee transition to the job, answer questions, and provide job guidance and training. Regular communication is critical to make sure both employee and employer are on the same page, and to discuss any potential barriers to performance. For example, if a big change is coming up, giving an early “heads up” and extra support during a transition is important.

Microsoft, Walgreens, and Freddie Mac are just a few of the larger companies that are recognizing the unique benefits of hiring individuals with autism. Additionally, more programs are being developed. For example, the Autism Employment Network, developed by Autism Speaks, uses LinkedIn as a networking platform for people with autism and employers. The Southwest Autism Research and Resource Center, which offers vocational and behavioral assessment, job matching, and on-the-job supports for adults with autism.
With an inclusive and supportive job environment, individuals with autism can thrive and contribute their knowledge, talent, and efforts and be an integral part of their community.
Teach Your Children About Autism
JCCHD | Sat, April 02, 2016 | [Autism Treatment][Community][Sibling Spotlight]Does your child have a friend who has autism? With 1 in 68 children having an autism diagnosis, the chances are high that your child has encountered or will encounter a peer who has autism at school, extracurricular activities, or community events. People with autism might behave and communicate differently. Here are some tips for helping your kids understand and accept their peers with autism and embrace those differences.

Photo by Stuart Seeger
Demystifying Differences
Being open and honest are keys to reducing the stigma of autism (as well as any other differences). Honest questions aren’t rude, and talking about autism can be done in a way that is educational and supportive rather than judgmental. If a child notices and asks or comments about differences they observe, validate their observation and help them understand. Avoid trying to quiet your child’s questions or encouraging them not to talk about it. When we show we are uncomfortable talking about someone’s different needs or behaviors, it sends the message that being different is shameful. If we can talk openly about it, the topic becomes routine, expected, and no longer something to avoid. Explain to your child that someone with autism may have a different way of communicating. Keep the conversation positive by focusing on what that person is able to do and why their differences are important, rather than stigmatizing them for all of the things they can’t or don’t do or the ways they aren’t the same as you or your child.
Being a Friend
What makes a friend? For most of us, friends are people who share some of our interests and who make us feel good when we’re around them, so we actively seek them out. If someone with autism is a friend to your child, teach them not to let his or her differences get in the way. Encourage your child to accept that differences make us who we are and to embrace these differences in everyone, not just individuals with autism. A great way to normalize this for your child is to model observation and acceptance of differences in your own friend group. Encourage your child to invite their friend to spend time with them, either alone or with a group of other people their age, but to consider their friend’s preferences. Some people might prefer one-on-one play dates or smaller groups, while others have fun with larger crowds. It never hurts (and often helps) to invite the person, regardless of the setting, but keep their needs and preferences in mind. Remind your child that not every friend has the same interests or likes the same things. When your child considers inviting their friend with autism, ask your child to remember anything in the environment that might be difficult for that person. For example, someone who is sensitive to loud noises might not enjoy a loud arcade, and someone with a limited diet might not find much to eat at some restaurants. Of course, your child can always give their friend the information and the choice, but let them know they should not to feel badly if their friend declines for these reasons.
Bullying
Some people with autism are targets for bullying. As a peer, there are things your child can do to help stop it. First, your child can defend the victim. As with any bullying or potentially dangerous situation, if any physical aggression is involved, your child should seek the help of a parent, teacher, or other adult. As much as we want to help a victim of bullying, it’s better that we stay safe by getting help than risk putting ourselves in the middle of danger. If the child with autism is being bullied in a non-physical way, having a peer come to his or her defense is one of the best ways to help. That defense can be standing up for the victim, or it can be as simple as being in the proximity of the victim so that he or she is no longer isolated. Extending an invitation to the victim to go to another location to remove him or her from the situation is another way to help.
Learning to be a friend to someone who seems different is a critical part of growing up. As parents and teachers, we play a huge role in providing information, guidance, and examples to teach our children to be kind, accepting, and supportive friends.
World Autism Day 2016 - Take the Action Pledge
JCCHD | Sat, April 02, 2016 | [Applied Behavior Analysis][Autism Treatment][Assessment Corner][Community][Events][Family and Food][Healthcare][News][Q and A ][Research][Resource Review][Sibling Spotlight][Staff Spotlight][Webinars]There are now well over 200 official “health awareness days” in the US, and many more unofficial ones. Autism is included on that list; April has served as Autism Awareness Month since the 1970’s, and April 2, 2016 is designated as World Autism Day.
Since more than two million people in the US have an autism diagnosis (and tens of millions worldwide), most people are now aware of autism. Most people know someone with autism and have heard about the skills, challenges, and needs of those in the community.
Awareness has helped bring these stories and issues to the forefront and continued awareness campaigns do help to keep the autism community, if even for a day, in the spotlight.
But we are aware. And with almost every day bringing about a new health awareness day, the spotlight shifts - yet the needs remain. So it is time to move beyond awareness and call for action.
It is a kind gesture when someone changes their social media profile for a day or shares an awareness post. And these gestures do raise the profile of the cause and the sponsoring organizations. But there are many things that we all can do that can have a profound and immediate impact on the lives of people with autism and their families.
So this April, we call for an Autism Action Month. Sign the pledge to do one or more of the following and have a direct and positive impact on the autism community:
* Include people with autism in your social gatherings
* Teach your children about autism
* Support employment for people with autism
* Participate in research to help advance the understanding and support of people with autism
* Donate to support programs for people with autism
* Promote programs for siblings of children with autism
* Promote programs for post-secondary education for people with autism
* Volunteer to support the local autism community
* Donate to support research in autism
* Advocate for appropriate health care coverage and rights for people with autism
This list is just the beginning, but if we use this month to make people aware of these needs and they pledge to take action on even one of them, it will be a huge step for the entire autism community.
So sign and share this petition today and help spread a call to action for autism!
The Health Benefits of Generosity
JCCHD | Tue, March 08, 2016 |Mahatma Gandhi once said, “The best way to find yourself is to lose yourself in the service of others.” One way to serve others is through generosity. Generosity is defined as the quality of being kind, understanding, unselfish, showing concern for others, or freely giving money, time, or other valuable things without expecting anything in return. Examples of this include making a charitable donation, spending time volunteering, or helping a friend with a task. Generosity not only has a positive impact on the person or organization one is helping, but it also has great health benefits for the giver.
Generosity can help lower your blood pressure, reduce risk of chronic disease, and reduce stress.
Chronic increased stress levels can lead to hypertension, or high blood pressure, and can contribute to chronic illnesses such as cardiovascular disease. But giving can help reduce stress, thus lowering your blood pressure. A 2013 study published in the journal Psychology and Aging found that volunteering regularly lowered the risk of hypertension in adults aged 51 – 91 years by forty percent. Another study published in the journal JAMA Pediatrics in 2013 found that volunteering lowered cholesterol and inflammation in adolescents. A group of high school sophomores were divided into two groups: one that volunteered for an hour each week for ten weeks, and one that did not volunteer at all. The students in the volunteering group were found to have lower cholesterol and inflammation at the end of the ten-week period than the students who did not volunteer. Thus, being generous can help lower hypertension and cortisol levels (a stress hormone). An article published in 2013 in the American Journal of Public Health also found that people who helped others were better protected against the negative impacts of stress.
Giving can boost your mood and make you happy!
Studies have shown that being generous can make you feel happy and increase life satisfaction. A 2008 study published in Science found that giving can make you happier. Forty-six randomly selected participants were given either $5 or $20 and assigned to spend the money on either themselves in the form of a desired item, expense, or bill, or on others, as a gift or charitable donation. They were called back in the evening and asked how they felt after spending the money as assigned. Those who spent the money on others felt much happier than those who spent it for personal use. Another study published in the Journal of Personality and Social Psychology in 2010 found that people felt better when they helped someone. One hundred thirty-eight college students were asked to keep a daily diary for two weeks reporting whether they had helped someone and how they felt. Most of them felt much better on days when they helped another person and/or did something for a good cause.
Generosity can help you make a social connection.
Helping others can help you make social connections and positively impact your relationships with people. You have surely heard the saying, “What goes around comes around.” This is absolutely true when it comes to generosity! Being a recipient of generosity inspires that recipient to give back to others, whether it be to the giver who directly helped them or to another individual or group. Giving builds a sense of trust and reliability, which leads to more social cooperation and connections. People are perceived as more positive and compassionate, which helps them feel closer to one another, thus establishing firm social connections.
Giving evokes gratitude.
Gratitude boosts positivity and your overall well-being, and giving can instill gratitude in a recipient. People who express gratitude are more likely to be optimistic and have a better outlook on life. Expressing gratitude to those around you or in your life can also promote healthy relationships and sense of connection. A way of expressing gratitude is to keep a daily gratitude journal, in which you write down everything you are grateful for each night before bed. This can bring a sense of content, satisfaction, and happiness.
Generosity can lead to a chain of people “paying it forward.” Paying a good deed forward entails doing something or giving somebody something without expecting anything in return. The recipient of the good deed is then inspired to do something kind for another person. There have been heartwarming news stories or social media posts about people paying it forward, such as paying for the order of the person in line behind them at a coffee shop drive-through, which ultimately inspires that person to pay for the following person’s drink and so forth. Studies show that generosity is paid forward to the third degree. For example, one person may give $20 to another person, who may give $10 to another individual, who may give $5 to another. Seeing others give or be generous is likely to cause somebody to also be generous.
It is clear to see that generosity is good not only for others, but especially for yourself. Being generous might be the most selfish thing you can do!
Feeling generous? Support The Johnson Center campaign at Amplify Austin and help support programs for people with autism and their families!
Navigating Higher Education for Students with Autism
JCCHD | Mon, February 22, 2016 |On Thursday, February 18th, Dr. Claire Schutte presented a webinar on Navigating Higher Education for Students with Autism. This webinar can be viewed here and there is a link to get a Certificate of Attendance after viewing here.
The most important point that Dr. Schutte made in her presentation was that it is possible for many people with autism to go on to some sort of college or postsecondary education program and it is important that we look at as many ways as possible to support them in this endeavor. Currently 1 in 3 people with autism pursues education after high school and with more support and programs that number could be higher.
Dr. Schutte’s webinar focused on four main areas: Planning, Options, Applying, and Supports.
- Planning: This is the first step toward seeking a successful postsecondary education. Dr. Schutte discussed the importance of focusing on REALITY:
When starting to plan for the post-high school program, one of the first areas to assess and program for are independent living skills. You can learn more about this here.
Some of this planning may take place during the ARD/IEP process in what is called Transition Planning. This should be a time to assess and teach all of the areas needed for a student to be successful in the school or program they are transitioning to after high school. This may include formal assessments (like the Strong Interest Inventory, the Campbell Interest and Skills Survey, or the Brigance Transition Skills Inventory) or informal assessments (like interviews with parents, teachers, and therapists, informal questionnaires, or observations).
Dr. Schutte recommends starting a binder specific to transition planning information where you can keep these assessments, any programs, goals, and school information.
- Options: Dr. Schutte reviewed ways to assess different schools and programs. Research can be done through school websites, conversations with other parents and students, Internet reviews, school counselors, visiting the schools and programs, and much more.
Making a list of what your student needs is a good place to start. There are many questions to consider, from location, program type, living options and more. Talking to the different programs and learning what services and supports are available is the best place to start to narrow your search.
- Applying: Once you have identified potential programs or schools, the application process can begin. Gathering documentation for test accommodations, test prep courses, filling out applications and gathering supporting documentation are all part of the process. An important consideration is whether or not to disclose any diagnosis during the application process. Dr. Schutte reviewed the options for both disclosure and non-disclosure.
- Support: There are many supports a student with autism can put in place and many ways to access them. Dr. Schutte reviewed many of these, including different offices and professionals who may offer support and many of the accommodations that can be made to help a student be successful.
There are several autism-specific programs that operate out of larger programs and universities and Dr. Schutte reviewed some of these during the webinar. If there are not programs in areas that you are looking, talk to your local university, community college, or technical college to see if an individual program with accommodations could be set up to support your student.
To learn more on this subject, watch Dr. Schutte’s webinar here. Later this year we will provide a webinar focused on ways postsecondary education programs can meet the needs of students with autism. For more information on this and our other webinars, follow The Johnson Center on Facebook or Twitter for the latest updates.
In the end, it is important to remember that the key to a successful transition to any program, whether a 4 year college, community college, technical school, or specialized program is assessment, planning, and preparation for the student, their family, and those who will be providing guidance and support.
Want to share a success story of a student with autism in college? Send to us email us at .(JavaScript must be enabled to view this email address) or you can share it on our Facebook or Twitter page with the hashtag #AutismAndCollege
Resources/References on Post-secondary Supports for Students with ASD
Websites
The Johnson Center YouTube channel
Autism Speaks postsecondary opportunities guide
Academic accommodations
CBS article on college programs specific to students on the autism spectrum
Training on accessing postsecondary education
Books
Baker, J. (2005). Preparing for Life: The Complete Guide for Transitioning to Adulthood for Those with Autism and Asperger’s Syndrome. Arlington, TX: Future Horizons.
Breakey, C. (2006). The Autism Spectrum and Further Education: A Guide to Good Practice. London: Jessica Kingsley publishers.
Grandin, T., Duff Y., K., and Attwood, T. (2004). Developing Talents: Careers for Individuals with Asperger Syndrome and High-Functioning Autism. Shawnee Mission, KS: AAPC.
Harpur, J., Lawlor, M., and Fitzgerald, M. (2005). Succeeding in College with Asperger’s Syndrome: A Student Guide. London: Jessica Kingsley Publishers.
Lawson, W. (2003). Build Your Own Life: A Self-Help Guide for Individuals with Asperger Syndrome. London: Jessica Kingsley Publishers.
Palmer, A. (2006). Realizing the College Dream with Autism or Asperger Syndrome: A Parent’s Guide to Student Success. London: Jessica Kingsley Publishers.
Thierfeld Brown, J., Wolf, L., King, L. & Bork, R. (2012). The Parent’s Guide to College for Students on the Autism Spectrum. Shawnee Mission, KS: AAPC.
Wehman, P., Datlow-Smith, M. & Shall, C. (2009). Autism and the Transition to Adulthood: Success Beyond the Classroom. Baltimore, MD: Brookes Publishing.
Articles
Shattuck, P., Narendorf Cooper B., Sterzing P., Wagner M., Taylor J. (2012). Postsecondary education and employment among youth with an autism spectrum disorder. Pediatrics;129 (6):1042-9.
Newman, L., Wagner, M., Knokey, A., Marder, C., Nagle, K., Shaver, D., Wei, X., Cameto, R., Contreras, E., Ferguson, K., Greene, S. & Schwarting, M. (2011). The Post-High School Outcomes of Young Adults With Disabilities up to 8 Years After High School. A Report From the National Longitudinal Transition Study-2 (NLTS2)(NCSER 2011-3005). Menlo Park, CA: SRI International. Available at http://www.nlts2.org/reports/
National Center for Educational Statistics. Postsecondary graduation rates (indicator 45-2012). 2012.
Sibling Spring Break Camp
JCCHD | Tue, February 09, 2016 |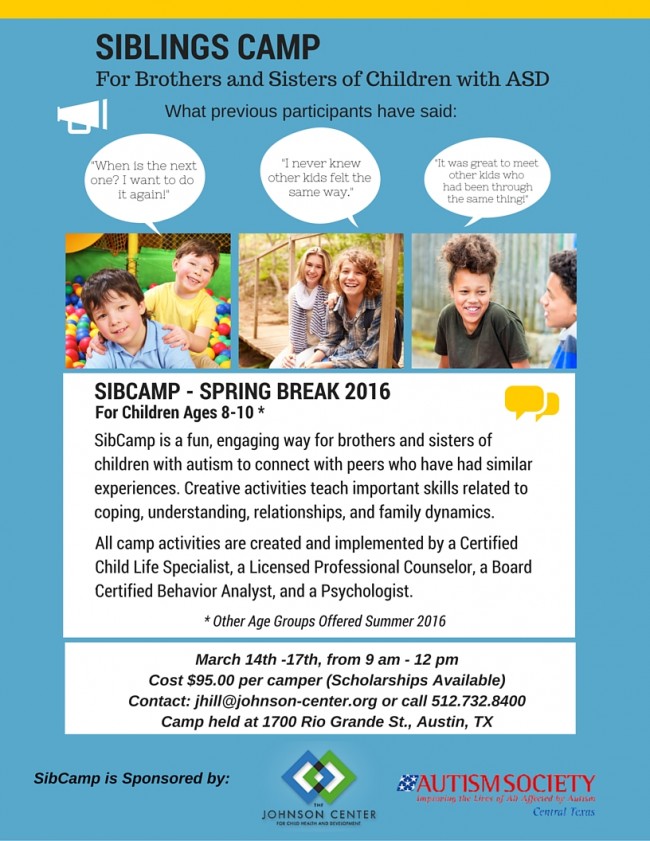
It’s King Cake Time!
JCCHD | Sun, January 31, 2016 | [Family and Food]King Cakes are an important part of the Mardi Gras tradition. This ring-shaped cake is as rich in history and tradition as it is in taste.
To read about the history of King Cakes, click here.
For people with food allergies or issues with certain foods, King Cakes are often something to be avoided. But we set out to make a King Cake that is free of gluten, dairy, soy, and rice. This recipe may also be adapted to be egg free. And it was given two-thumbs up by our taste testers. So put on some Mardi Gras Mambo and make a treat to celebrate the season.
KING CAKE
INGREDIENTS
Dough:
• 3½ cups gluten free flour blend (You can use Bob’s Red Mill All Purpose Gluten Free Flour or the custom blend below*)
• ½ cup tapioca starch
• 1 Tbsp (1 packet) rapid rise yeast
• 3 Tbsp sugar
• ½ tsp salt
• 3 tsp ground flaxseed
• 1 Tbsp hot water
• 1 tsp baking powder
• 3 Tbsp Earth Balance Soy Free “Buttery” Sticks
• ½ cup water
• ½ cup dairy free milk (We used unsweetened coconut milk)
• 2 eggs, at room temperature
• 1 tsp cider vinegar
• 2 Tbsp coconut oil
• 1 tsp vanilla extract
• ½ tsp almond extract
* NOTE FOR CUSTOM FLOUR BLEND:
2 cups Millet flour, 2 cups Amaranth flour, 1⅓ cups potato starch (not flour), ⅔ cup tapioca starch. Combine in a zipper lock plastic bag, shake to mix.
Filling Ingredients:
• 8 ounces Daiya dairy-free cream cheese, softened
• ½ cup packed brown sugar
• 1 Tbsp ground cinnamon
• ¾ cup finely chopped pecans
Egg wash
• 1 egg white
• 1 Tbsp water
Icing
• 1½ cups confectioners’ sugar
• ½ tsp vanilla extract
• 1-2 Tbsp coconut or almond milk – add until you get desired consistency
• Purple, Yellow, and Green sugar sprinkles (India Tree makes sprinkles colored with natural flavors)
INSTRUCTIONS
1. Mix first five dry ingredients until combined. Set aside.
2. In a glass measuring cup, add ½ cup water and Earth Balance and microwave until just melted. In small bowl combine ground flax seed and hot water.
3. Stir in all wet ingredients and flax seed mixture with the dry.
4. Put down a non-slip mat or dampen your counter top and put down a piece of plastic wrap so that it covers an area bigger than 8"x16”. To avoid sticky dough, spray some oil onto the plastic wrap, than sprinkle with about 2 Tbsp of sugar. Knead dough into a ball and lay on plastic wrap - cover with another piece of plastic wrap sprayed with oil. Roll the dough out to approximately 10"x18”. Remove the plastic wrap.
5. Mix dairy free cream cheese, brown sugar, and cinnamon together in a medium mixing bowl until thoroughly combined.
6. With a spatula, spread the filling mixture evenly onto dough, leaving an inch around the edge without any filling. Evenly sprinkle pecans over filling.
7. Prepare a baking sheet with parchment paper or a Silpat and set right next to your dough. Carefully along the long end, start rolling it up into a long cylinder (sprinkle with extra flour if needed). Using the plastic wrap, lift the roll onto your baking sheet and placing it on its side. Remove the plastic wrap and gently form the roll into a circle and pinch the ends together.
8. Whisk egg wash ingredients together. Using a pastry brush, brush top of cake. Cover loosely with plastic wrap and let it rise in a warm place for 30-40 minutes until nearly doubled in size.
9. Preheat oven to 350. Bake for 30-35 minutes.
10. Take out of oven and let sit for 10 minutes. Carefully move to cooling rack.
11. Mix icing ingredients together and drizzle icing onto top of cake. When cool, cover top of cake in thirds with purple, yellow, and green sprinkles.
12. Optional: Insert a bean or baby in the bottom of the cake to determine who gets to make the next King Cake!

Notes: Adapted from saltedplains.com
2015 Halloween Hoot
JCCHD | Wed, October 07, 2015 |
Fall 2015 Social Skills Group
JCCHD | Tue, August 25, 2015 |
GrapeUp! Come Together! - Gardening Fun
JCCHD | Fri, August 21, 2015 |
GrapeUp! Come Together! - Sandwich Art
JCCHD | Wed, August 12, 2015 |Saturday, July 25, was full of good food and great fun. We learned all about nutrition at the Grape Up! event dedicated to making Sandwich Art.
We started off the day with a fun story called “The Giant Jam Sandwich,” by John Vernon Lord, read by our presenter for the day, Zabin. Our ASL and Spanish interpreters helped us tell the story.
Zabin, a research assistant at the Johnson Center, then told us a little bit about the nutrition in the foods we eat and how to best fuel our working bodies. We learned what was truly healthy, like fruits and veggies and whole grains, what foods we should eat in moderation, like peanut butter and avocados, and what we should try and limit, like ice cream and cookies.
We got to get up and get moving by playing a red-light, green-light game with healthy foods to signal “go” and unhealthy foods for “stop.” It was a fun way to practice what we learned about nutrition.
The coolest part of the day was when we got to make our own sandwich art out of sun butter and jam sandwiches. We got to decorate them any way we wanted. There were cookie cutters to make different shapes, lots of little snacks to decorate with, and plenty of food for everyone. Who knew sandwiches could look as yummy as they taste? We had Glutino pretzel snack bags and Oh So! Organic juice pouches to go with the amazing creations.
Everyone then got to make their own fish bowl, using glitter, stickers, and gluten-free cereal as aquarium rocks.
Amy, our photographer, took lots of pictures of all the fun and of the beautiful sandwiches we made. Our wonderful volunteers helped with the sandwich art and the crafts so that parents were able to enjoy their morning with some coffee, donuts, and a chance to relax.
It was a fun, delicious morning. If you want to learn more about sandwich art, check out one of our amazing Nutrition Department interns, Sarah, who got the chance to demonstrate sandwich art on the show Studio 512.
Photo Credit Amy Zhang
GrapeUp! Come Together! - Yoga
JCCHD | Wed, August 12, 2015 |
Back to School Bash 2015
JCCHD | Mon, August 10, 2015 |Mark your calendars! Our annual Back to School Bash is coming up and this will be the best year ever. With support from our sponsors Vintage IT Services and Sogeti there will be free fun for the entire family and everyone is invited to attend.
Come out and enjoy fun and games, music, a bounce house, allergen-friendly foods, a family photo booth and more. The first 50 attendees will get a Back to School bag loaded up with great school supplies! There will be LOTS of prizes to be raffled off (including gift certificates to local restaurants, family activities, and more) so be sure to mark your calendars.
Music by Lucas Miller, the Singing Zoologist, and Zumba fun by Austin Zumba.

SIbCamp in August
JCCHD | Mon, August 03, 2015 |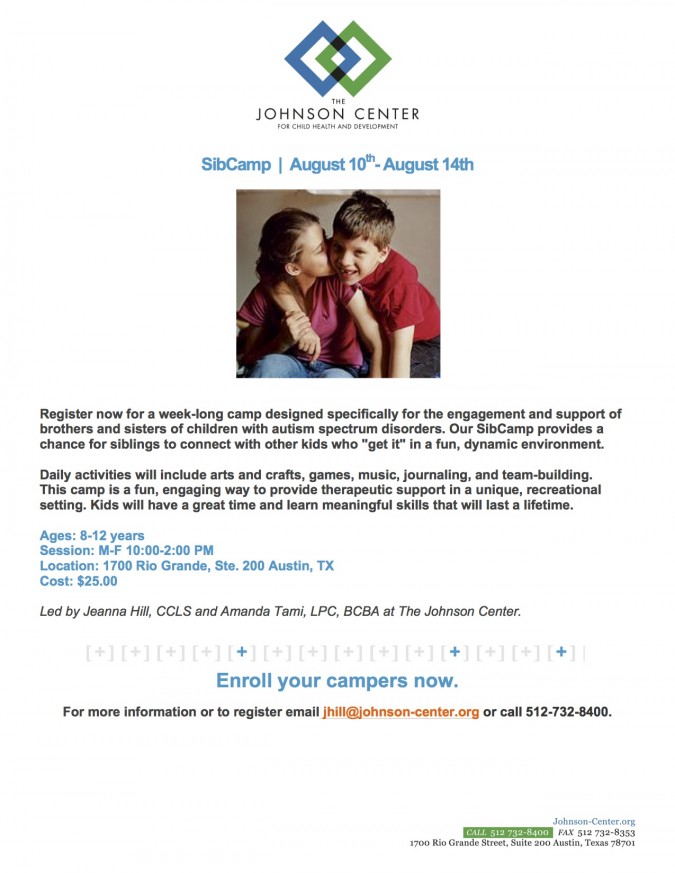
GrapeUp! Come Together! - Be A Junior Weatherperson
JCCHD | Thu, July 30, 2015 |
GrapeUp! Come Together! - Why is The Johnson Center hosting inclusive recreational events?
JCCHD | Mon, July 27, 2015 |It has been said that prejudice rarely survives experience. Once we come together and see people as they are—interesting, flawed, funny, curious, intriguing, smart, challenged, strong, human—then we are able to see the characteristics we share, we aspire to have, we complement, we can learn from, and we can support.
This is the premise behind the “Grape Up! Come Together!” events, hosted by The Johnson Center for Child Health and Development.
All children benefit from inclusion. There are numerous studies that support this—not just children with special needs, but everyone. Including people of all abilities, backgrounds, and experiences is how we expand our own perspectives and learn to engage and appreciate people who have experiences different from our own. And that is how we build strong, compassionate, engaged communities.
At “Grape Up!” events everyone is invited, everyone belongs, and everyone benefits. Our staff, volunteers, and special guests work hard to ensure every child who attends has fun, is included, and is recognized for the gifts they bring to the gathering. Accommodations are provided to make certain that this takes place. These include sign language interpreters, Spanish-language interpreters, visual schedules, accessible spaces, low child-to-staff/volunteer ratios to ensure assistance is available, and prepared modifications for games or crafts.
For children who do not need these accommodations, the benefits are simple: they have a fun time, make new friends, and learn to appreciate diversity. Understanding and respect are at the core of any opportunity for children of differing abilities and cultures to learn and have fun together.
So bring your children and join a compassionate bunch at “Grape Up! Come Together!” Because what could be better than kids having fun while playing and learning together?

GrapeUp! Come Together! - We All Scream for Ice Cream!
JCCHD | Thu, July 23, 2015 |On Saturday, July 11, Pease Elementary playground was the place to be. The Johnson Center staff and volunteers got there early and worked hard to get set up for the fifth “Grape Up! Come Together!” event. This was the day we learned about and celebrated all things ice cream!

We started off the morning by learning how to make ice cream at home with a special ice cream ball. We added non-dairy coconut creamer, rock salt, sugar, and ice to the ball, and we were all set to make delicious ice cream! We had to shake, shake, shake the ice cream ball. We passed it through the audience and everyone took a turn shaking it. We had plenty of volunteers, so parents got the chance to sit back and relax with a cup of complimentary coffee (but we also got them in on the fun and they helped to shake too).


Sarah the Human Ice Cream Cone then read us the story of two best friends and a cone of ice cream called “Should I Share My Ice Cream?” Our great team of American Sign Language interpreters and our Spanish interpreter were all on hand to translate as the story was read. We all learned the sign for ice cream, and that the best way to eat ice cream is to share it!

Finally it was time for the magic to happen: together we built a 20-foot ice cream sundae. Amy’s Ice Cream generously donated 150 scoops of non-dairy strawberry, aloha, and peach ices for this event.

The children built the sundae with lots of bananas, cookie crumbs, granola, cherries, and whipped coconut cream - yum! So that ALL our friends could join in the fun, all the ingredients were gluten-free, casein-free, and nut-free.
We had some helpers who got to run up and down the sundae adding rice whip and chocolate sauce. Then the countdown began… 10.9.8.7.6.5.4.3.2.1……


Everyone ran with a spoon to dig in. The sundae was so delicious!
We ended the day by making our own paper ice cream cone craft to take home with us. We definitely love glitter and ice cream.

We wrapped up with snack time. This week we had an allergen-friendly KIND bar and OH-SO Organic juice box. The kids took lots of pictures with Sarah the Ice Cream Cone.

We were so lucky to meet so many new friends and families, and we hope more will come join us as the summer continues. Join us each Saturday morning for more fun. We would love to see all of you there!
Photos Courtesy of Amy Zhang
What Every Child Needs to Know About Dog Safety
JCCHD | Wed, July 22, 2015 |On Saturday, July 18th, The Johnson Center for Child Health & Development had the pleasure of hosting a workshop for kids presented by canine-behavior expert Caitlin Lane, CPDT-KA (Certified Professional Dog Trainer – Knowledge Assessed) from Austin Dog Zone.
In between fun games, a photo booth, story time, and animal crafts, the kids learned proper etiquette and safety tips for approaching and playing with dogs. This is important information for all children to know and practice to ensure their safety at home and in the community.
Caitlin began by explaining that many dogs are friendly, but if you are approached by a dog who makes you scared or uncomfortable, the first thing you should do is to “become a tree.” And how does a person become a tree? You stand with your feet firm (“rooted” in the ground), your arms crossed down in front of you, perfectly still, looking down at the ground. This will confuse the dog and he will most likely leave you alone.
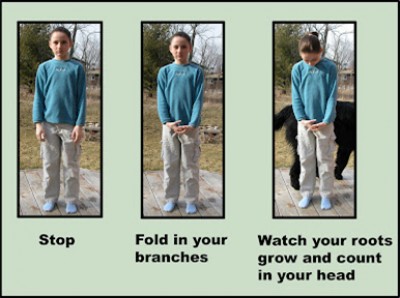
Photo Credit Be-A-Tree.com
If you get knocked over or are already on the ground during this encounter, you should “become a rock.” You can become a rock by curling over with your knees tucked underneath you, facing the ground, with your hands covering your neck, and keeping as still as possible.

Photo Credit DogGoneSafe.com
The kids practiced this throughout the presentation – every time Caitlin would hold up the picture of a snarling dog, the kids would assume the tree or rock position. This practice will help ensure they can employ this skill in the event of an emergency.
Caitlin then went through the steps of how to tell if a dog is friendly and approachable. Caitlin taught the children that we can use our bodies to see if the dog is ready to meet us or not.
Eyes: Use your eyes to look at the dog to see what signs are being given. Does the dog have an open mouth with a panting tongue? This is an indication of a dog ready to play. Is the tail of the dog down and relaxed? This is another sign of an approachable dog. However, if the dog’s mouth is closed, if the ears are back, or the tail is straight up, this indicates the dog is worried or scared and should not be approaced. Another sign of a dog who should be left alone is the “whale” eye, or when you can see the whites around the eye of the dog. If you see a dog begin to yawn (when you know it isn’t tired) or if the dog licks around its mouth and isn’t around food, these are signs the dog is stressed and should be left alone.

Happy Dog Photo Credit Themes.com
Worried Dog Photo Credit MooseysCountryGarden.com
Mouth: Use your mouth to ask your parents if you may approach the dog. If they say yes, use your mouth to ask the dog’s owner if you may approach the dog. If they say no, then you can’t approach the dog. If they say yes, then you can proceed with these steps.
Hands: Use your hand, balled up into a fist, to invite the dog to meet you. Squeeze your hand into a fist and hold it out in front of you. Let the dog come up to smell your fist. But wait for the dog, don’t shove your fist in its face. Put your fist down and low where the dog can check you out. If the dog sniffs your fist and stays near you, then you may pet the dog on the back of the neck or scratch behind their ears. Dogs don’t like hugs or kisses like people do, so show them you like them by respecting their space and giving them the attention they like – scratches on the shoulder area and pats.
Legs: If you encounter a dog who is tied up and can’t get away, don’t approach it. This isn’t fair to the dog. It may feel trapped or scared, and when dogs are trapped and scared they are more likely to bite. So if you come across a dog who is tied up, who demonstrates any of the stress signs listed above, or an owner who says no when you ask if you can pet their dog, then use your legs to walk away.
It is a good idea to practice theses steps with a known, friendly dog to ensure your child has safe habits when it comes to canine encounters. For more information visit Doggone Safe for great tips and photos to help discuss and review this information with your kids. Another great resource with terrific videos is The Family Dog. If your child benefits from using visual cues, watch the videos, then print the photos and make a game of practicing these responses and steps. You can begin by playing pretend, where you are the dog and the child approaches you.
Dogs have long been known to be man’s best friend…now let’s teach our kids to safely be a dog’s best friend.
GrapeUp! Come Together! - Sandwich Art
JCCHD | Tue, July 21, 2015 |
GrapeUp! Come Together! - Making Music
JCCHD | Tue, July 21, 2015 |On June 27th we had a crazy Saturday full of music with the Johnson Center at the Pease Elementary playground. It was the Johnson Center’s fourth “Grape Up! Come Together!” event in our summer series, and we had a blast. This week Lauren. a very special guest from the TexARTS Association, taught us all about music and instruments. Lauren read us the book My Family Plays Music by Judy Cox and showed us all the different instruments in the story, like triangles, tambourines, and drums. Our team of American Sign Language interpreters and our Spanish interpreter translated the story as it was read.


Afterward, Lauren and her duet partner Corey taught us a short song and we all got to sing along together.

We then got to make our very own instrument shakers out of paper towel rolls, beans, rice, and lots of glitter. Everyone had a lot of fun making music and shaking them around.


The parents who were there got to learn about child safety, making these cool pamphlets with their children’s fingerprints in them in case they are ever separated.
Next came the music parade for which we all picked out our favorite instrument from the huge box of instruments. There were maracas, xylophones, clackers, and shakers—even an accordion! Once we all had an instrument, we got to march around the playground, playing our song.



To wind things down everyone got to write their own story music book, where we practiced writing and using nouns, verbs, and adjectives. Since there were so many awesome volunteers who worked one-on-one with the children on the crafts and books, parents got to sit nearby and relax with complimentary coffee and snacks.
Everyone had fun in the photo booth, taking silly pictures with our photographer. And, as always, we had an allergen-friendly snack at the end of the event. This week we had KIND bars and OH-SO Organic juice.
We had a great turnout and lots of fun, and we hope to see even more families in the next couple of weeks as our summer series continues with more activities and fun!
GrapeUp! Come Together! - All About Animals
JCCHD | Mon, July 13, 2015 |
Help us buld a 20’ Ice Cream Sundae
JCCHD | Fri, July 10, 2015 |
Navigating Insurance: The Appeals Process
JCCHD | Tue, June 30, 2015 | [Autism Treatment]In our recent webinar Understanding and Optimizing Your Health Insurance Coverage: What Every Parent Needs To Know, we discussed information regarding what to do in the event that your claim to your insurance company is denied. This is called the Standard Appeals Process.
It is not unusual that you will file a claim for a service that is initially denied by your insurance. There is a fairly simple process to appeal this decision.

Most insurance carriers have specific forms that are required to process an appeal. These are typically found on your insurance carriers website (there is usually a section titled “Forms”). If you don’t have access to the website, call their Customer Service line and ask a representative to send you the forms.
Try to submit as much information as possible to support your request for an appeal. Documentation from your clinician is often helpful. Be sure to read the reasons for the denial on the Explanation of Benefits that your carrier will have provided to you so that you are sure to answer any outstanding questions or misinformation they may have.
Almost all insurance policies outline the time frame for submitting an appeal and for receiving responses from the carrier.
Watch the webinar to learn more about the levels of appeals, how to expedite an appeal in an urgent situation, tips on how to write an effective appeal letter, why you should include published research related to your appeal, and when there is no value in appealing.
Insurance companies do reverse their decisions on appeals, so it is important to understand the process if you have been denied.
GrapeUp! Week 3 - All About Bees!
Sarah Song, GrapeUp! Intern | Thu, June 25, 2015 |This past Saturday, June 20th, we got to learn all about bees at The Johnson Center’s third fantastic Grape Up! Come Together! event.
This week, Sarah the Bee read Bee and Me by Elle McGuinness. We had our team of American Sign Language interpreters, as well as a Spanish interpreter, who translated as the story was read. Travis taught us all how to sign the word “bee”!
We were so lucky to have our own beekeeper, Brandon, from Austin Bees come out to show the kids some bee keeping equipment and answer all of their questions about bees. We learned so much, from bee safety to the bee waggle dance!

After the talk, Sarah the Bee led the newly appointed Little Beekeepers around the playground on a pollination hunt. The kids go to help help “pollinate” the pretty flowers by taking sparkly pieces of “pollen” from one flower to the next.

Then the kids got to make their own bees with paper towel rolls, googly eyes, and pipe cleaners. They looked fantastic!

Everyone even got to write their own bee book (and practiced using our nouns, verbs, and adjectives).

Once again we were lucky enough to have plenty of volunteers so that parents and caregivers were able relax and enjoy the complimentary coffee. And of course, the little beekeepers enjoyed their complimentary snacks (thank you, KIND!).

We had a great turn out and lots of fun!

We hope to see even more families next Saturday, June 27th, when we will be making musical instruments. Come join our band! Click here for more information about Grape Up! Come Together!
GrapeUp! Week 2 - Fairy House Fun
Sarah Song, GrapeUp! Intern | Thu, June 25, 2015 |On Saturday, June 13, the staff from The Johnson Center was joined by over fifty fairies-in-training at Pease Elementary School for another successful Grape Up! Come Together! event.
Fairy Tiffany read from Olivia and the Fairy Princesses by Ian Falconer. We had a team of American Sign Language interpreters, as well as a Spanish interpreter, who translated as the story was read. We even had a giant version of the book so everyone could read along.

We even learned how to say “fairy” in sign language!
We loved our magical fairy theme! The kids searched around the school yard, led by Fairy Tiffany, hunting for secret, magical fairy houses. We found four REAL fairy houses!

One fairy was getting ready for a tea party and had cake already set out on the table!

The fairies-in-training then got to build their very own magical fairy houses, with lots of glitter, markers, leaves, moss, and flowers.

Before everyone flew away, the kids got to write their own fairy storybook, with a little practice using nouns, verbs, and adjectives.

There were lots of volunteers on hand to help, so the parents of the fairies-in-training got to sit back and rest with complimentary coffee while their little ones had a great time!
Everyone enjoyed a KIND bar and juice box for a snack while waiting to take their picture with Fairy Tiffany.

We hope to see even more families as our summer series continues. Click here for the full schedule.
Navigating Insurance: Filing An Out-of-Network Claim
JCCHD | Thu, June 25, 2015 | [Autism Treatment]In our recent webinar, Understanding and Optimizing Your Health Insurance Coverage: What Every Parent Needs To Know, we outlined how to file an out-of-network claim.
We provided step-by-step instructions on filing the claim that are simple to follow, such as:
- You will receive a receipt from your doctor or clinic after you have checked out and paid for your service. Make a copy of this – one for your records and one to submit.
- Go to your insurance carrier’s website, find their “Forms” section, and print out a claim form.
- You will use the receipt from the clinic to find the coding information requested on the claim form. Fill out the claim form completely. Make a copy - one for your records and one to submit.
- Attach the receipt to the claim form and mail it to the claims address listed on the claim form.
Watch the webinar for important information like how long insurance companies typically have to process a claim, and tips on how to keep your claim records organized.
GrapeUp! Week 1 - A Scavenger Hunt
Sarah Song, GrapeUp! Intern | Thu, June 25, 2015 |On Saturday, June 6, 2015, The Johnson Center presented Grape Up! Come Together! to the Austin community for the first time.

Gathered at Pease Elementary School, we had our very own Grapelet (Office Manager Tiffany) read from Waylon and Stogie in The Scavenger Hunt, by Mark Pendergrass. We had a team of American Sign Language interpreters, as well as a Spanish interpreter, on hand to make sure everyone was able to enjoy the story. We also had a GIANT version of the book to follow along as we read it.

We had an absolute blast with our pirate and scavenger hunt theme! The kids were able to go on an interactive scavenger hunt around the Pease Playground. We looked for feathers and rocks and all things shiny and soft, with Pirate Betsy leading the way. At the end of the hunt, all the kids found their treasure and were able to take home a pirate prize.

During snack time, everyone enjoyed their delicious KIND bars and juice boxes before we moved on to our pirate themed photos!

We had a great turn out and lots of fun! We hope to see even more families join us as our summer series continues with more activities and fun!
GrapeUp! Come Together! June 27,2015
JCCHD | Thu, June 25, 2015 | [Community][Events][News][Sibling Spotlight]
Documenting Insurance Company Communications – A Worksheet
JCCHD | Thu, June 25, 2015 | [Autism Treatment]In our webinar Understanding and Optimizing Your Health Insurance Coverage: What Every Parent Needs To Know, we provided a link to a very helpful step-by-step worksheet. Before you pick up the phone to call your insurance company to inquire about your coverage, you’ll want to have this worksheet in front of you and a pen ready. Getting all of your information is much easier if you follow the worksheet questions. The worksheet is also a great way to stay organized—it has the who, where, what, and when details of the insurance phone calls so that you can document and file them for future reference.
The worksheet asks for the relevant information: the Practitioner NPI (National Provider Identifier) number, the clinic tax ID number, credentials, and clinic address, and all the details that your insurance representative will likely ask you. There are boxes to check if the services are in- or out-of-network, as well as space to write the name of any specific representative who may be assigned to you on an on- going basis. If you are an existing patient, it is possible that your clinic will be able provide the CPT codes that describe the service you are pursuing, which will aid in confirming coverage. Every worksheet has reminders to note the name of the insurance representative you are talking to and the date and the time of day, in addition to the all-important Call Reference Number.
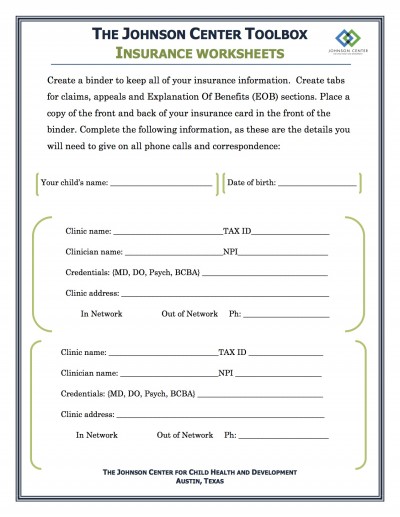
Many important reminders are included and easy to check off: is there a ceiling (maximum) on the number of this type of appointment allowed in your policy? Have you met your deductible? At what % is this appointment going to be reimbursed? What is the co-pay? Does the practitioner need a specific credential for it to be covered? Does it need pre-authorization? How many days does insurance have to provide a reimbursement check to you?
Once you’ve made your insurance call and your worksheet is complete, file it in your insurance binder. You can mark your calendar to follow up on reimbursement checks and use the details of the worksheet to appeal a claim if needed.
The full worksheet is available on our website at:
http://www.johnson-center.org//downloads/pdfs/2015_insurance_worksheet.pdf
Pre-Authorizations and Insurance: What You Need To Know
JCCHD | Thu, June 04, 2015 | [Autism Treatment]In our NAVIGATING INSURANCE webinar on May 21st, we discussed the Pre-Authorization process [sometimes called Pre-Certification]. Many insurance companies require pre-authorization to help determine whether a proposed treatment plan is necessary. We suggest you call your insurance company prior to any specialty or out-of-network clinical visit. This is especially important if you are starting an intervention that is specialized (such as a Feeding Clinic) or recurring (like speech therapy). If any services are performed prior to gaining pre-authorization it may result in you being financially responsible for all or part of the cost of the services.
Let’s say your physician and therapy team determine that a behaviorally-based Feeding Clinic is critical for your child’s development and progression. The Feeding Clinic is projected to last 5 days with 3 two-hour meals daily (6 hours of ABA x 5 days = 30 hours, plus parent training time). Even if your insurance is covering ABA services on an ongoing basis, it is prudent to get a pre-authorization for the specialized Feeding Clinic.

Pre-authorization forms must be completed and sent with statements of necessity from the prescribing clinician. Sometimes your clinician will submit the forms on your behalf. For the sake of expediency, you may need to gather information and documents from various clinicians to submit the pre-authorization request on your own. You will then wait for confirmation in writing that insurance will cover this service before you begin. Typically, insurance carriers must respond to a pre-authorization request within 30 business days. Be sure to use the Insurance Worksheets on all of your calls and keep copies of all the paperwork in your insurance binder. Mark the date on your calendar to call about the verdict!
Here’s the typical pre-authorization process for insurance companies:
• A member or provider will make the request for pre-authorization in writing and submit all necessary records to the insurance company. When a member goes to a non-network physician, it is the member’s responsibility to obtain pre-authorization.
• A Clinical Coverage Review Department then makes coverage decisions for pre-authorization, based on the submitted medical record information.
• Once a provider or member submits a request, the insurance company typically makes a decision within three business days. The decision could take up to 15 days if the provider or member does not initially submit all necessary information to make a determination. For urgent requests, the insurance company usually makes a decision within 24 hours.
• An appropriate reviewer, such as a board-certified physician or specialist, makes the final determination on all denials.
• A copy of the decision is faxed or mailed to the provider and mailed to the member.
• In the event that coverage for a requested procedure, drug, or service is denied, members have the right to appeal, as outlined in their plan documents.
File all your paperwork on the pre-authorization approval in your insurance binder, as your clinician may need approval codes or reference numbers from these documents during their billing process.
And remember, if needed, you can always appeal a pre-authorization denial!
Explaining the Explanation of Benefits Form
JCCHD | Thu, June 04, 2015 |How on earth do you read an EXPLANATION OF BENEFITS statement? In our webinar, NAVIGATING INSURANCE, we discussed the Explanation of Benefits (EOB) document provided by your insurance company. The document outlines how benefits were paid out for a specific claim. For in-network services, the EOB will arrive after your care provider has processed your claim. The EOB explains the charges, what the insurance company paid, what they denied (and why), and if you should expect to have an outstanding bill with the provider. It is important to remember that you do not pay the EOB, it is a statement, not a bill.

For out-of-network services, you will most likely pay your clinician at the time of service (unless other arrangements have been made). Once you submit your receipt showing what you paid and a completed claim form to your insurance company, they will send you an EOB. The EOB will arrive with a reimbursement check or a statement explaining the reason they are denying reimbursement.
It’s important to double-check that the information on the EOB is correct. Be sure to check the following:
• The date of service
• CPT code
• The amount allowed for the appointment
• Any amount applied to your deductible
• Any co-pay reported
• What, if anything, they paid directly to your provider
• The patient’s responsibility (amount they have determined you owe)
The notes section will list the reason for the amount of your reimbursement check or the reason for the denial of reimbursement. Often the explanation for denial of services is one that you can appeal; for example, it may state something like: *charges for speech therapy are only covered when therapy is expected to restore speech function or correct a speech impairment from non-chronic conditions, acute illnesses, or injury…
An appeal is typically a one-page form that your carrier will provide. You can send it in with notes from your therapist or clinician to support your claim that your insurance policy should cover the service. This is the point when you will be happy you took such detailed notes while on the phone with your insurance company [download our Insurance Call Worksheet here]. In the event that the denial is for a reason you were previously told was covered, you will have documented all the important information. You can use this, including the call reference numbers, to whom you spoke, services they promised, etc., in any appeal information you submit.
Even if the representative told you up front that this was not a covered service, you may still appeal with your clinician’s support and documentation. Insurance companies will typically send the appeal to a review team and will return with a decision, typically within 30 business days. Preparing and lodging an appeal can be fairly quick and it never hurts to be a squeaky wheel with insurance companies!
In-Network versus Out-of-Network Coverage....What's the Difference?
JCCHD | Tue, June 02, 2015 | [Autism Treatment]In our recent webinar, NAVIGATING INSURANCE, we discussed the difference between in-network and out-of-network insurance services. In-network coverage is when your insurer negotiates with a wide range of doctors, specialists, hospitals, labs, and pharmacies to pay a set price for services. These are then the providers in your “network.” Your insurance provider will typically pay a higher percentage of your claim if you go to in-network clinicians. Typically you will have a set co-pay to see in-network providers, and those providers agree to only charge you those set rates.
You may find that you need to see specialists who are outside of your network. Many times, patients will travel to different cities and states to find a specialist for their particular needs. Sometimes the specialty clinics are not contracted with any insurance carriers and the patient (or their parents/caregivers) pay the full amount at the time of service. Many insurance policies will cover out-of-network providers, but they have not agreed to any set rates and they will sometimes only pay a percentage of the costs. Your plan may require higher co-pays, deductibles, and co-insurance for out-of-network care.
It’s less common that your plan will not cover out-of-network care at all, leaving you to pay the full cost yourself. It’s imperative that you check with your insurance carrier prior to any clinical visit to understand the coverage your insurer provides, whether it’s in-network or out-of-network.
Following is an example that outlines how the same appointment is billed differently, depending on the in-network or out-of-network coverage. Do your homework and you’ll know what to expect from your insurance policy!
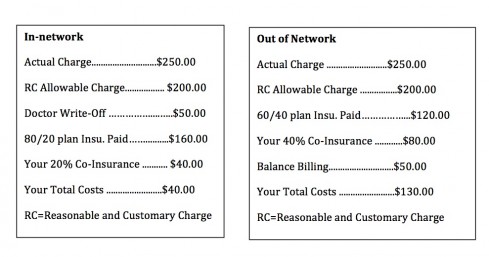
Understanding Insurance Language
JCCHD | Mon, June 01, 2015 |A Parent’s Guide to Navigating Insurance Coverage teaches you the language of insurance and gives you the tools you need to cut through the fine print and understand your coverage. In this webinar we discussed a glossary of terms that will help you navigate conversations with insurance company personnel and read insurance paperwork. Below is a review of those terms:

In-network: Your insurer negotiates with a wide range of doctors, specialists, hospitals, labs, and pharmacies to pay a set price. These are the providers in your “network.” Your insurance provider will typically pay a higher percentage of your claim if you choose an in-network provider.
Out-of-network (OON): Providers who are outside your network who have not agreed to any set rates with your insurance company. Your plan may require higher co-pays, deductibles, and co-insurance for out-of-network care. Your plan may not cover out-of-network care at all, leaving you to pay the full cost yourself. Also, if you go to an OON provider, you may be responsible for paying you bill in full and submitting claim paperwork yourself to receive reimbursement from your insurance company.
Co-payment: A specific charge for a medical service or supply. Typically, a “co-pay” is charged at the time of an office visit or purchase. For example, your insurance may require a $15 co-payment for an office visit or brand-name prescription drug, after which the insurance company often pays the remainder of the charges.
Co-insurance: The amount you are required to pay for covered medical services after you’ve satisfied any co-payment or deductible. For example, if your insurance company covers 80% of the cost of a specific service, you will be required to cover the remaining 20% as co-insurance.
Annual Maximum: Maximum dollar amount your insurance will pay in a contract year. There may be separate maximums for specific services like ABA, medical visits, diagnostics, etc. Your policy may also limit services by number of visits per contract year.
Contract year: The time frame of your coverage. This may be Jan-Dec or any period of 12 months, depending on your policy.
Reasonable & Customary Charges: The dollar amount an insurance carrier is willing to pay for a specific service. Insurance companies can determine this based on your geographic location. Often times they use the reimbursement rate that Medicaid uses. Reasonable and Customary charges affect your payment amount when you go out-of-network. For example: a chest X-ray at your Out-Of-Network doctor may cost $120, but your insurance carrier may determine the reasonable & customary charge to be $100. In that case, you would be required to pay the $20 difference.
Diagnosis codes: A 3-digit code (may include additional decimals) used to group and identify diseases, disorders, symptoms, poisonings, adverse effects of drugs & chemicals, injuries, and other reasons for patient encounters. Example: 249.00 is the diagnosis code for diabetes.
Procedure/Current Procedural Terminology (CPT) code: A 5-digit code used to identify a specific clinical service. For example, there is a diagnosis code for a broken leg. The procedure code or CPT code is for the service of putting a cast on the broken leg. IMPORTANT: Both diagnosis codes and CPT codes can only be determined by qualified clinicians. To change a code on a claim without the approval of a licensed clinician is insurance fraud.
Explanation of Benefits (EOB): a document provided by your insurance company outlining how benefits were paid out for a specific claim. If your appointment is In-network the EOB will arrive after your care provider has processed the claim, possibly before your bill arrives. If you chose to go Out-Of-Network, the EOB will arrive after you have paid your clinician and submitted your receipt for reimbursement. The EOB may be accompanied by a reimbursement check or an explanation for their refusal to reimburse you.
Pre-authorization: A decision by your insurer that a health care service, treatment plan, prescription drug, or durable medical equipment is medically necessary. This is sometimes called prior authorization, prior approval, or pre-certification. Your insurance company may require pre-authorization for certain services before you receive them, except in an emergency.
These terms should help you when talking with your insurance company or benefits coordinator about your coverage.
Navigating Insurance: Types of Insurance
JCCHD | Thu, May 28, 2015 | [Autism Treatment]We believe that informed consumers are powerful advocates. Over the last ten years, we have often heard patients, parents, and caregivers express confusion and dissatisfaction with their experiences with their insurance carriers. Our administrative staff has put together a webinar to help you understand the ins and outs of health insurance from a consumer’s perspective.
The webinar, A Parent’s Guide to Navigating Insurance Coverage, can be viewed here. Based on your questions and requests for more information, we are providing a follow-up blog series to expand on the information in the presentation.
One of the first things we reviewed in the presentation was the language of insurance and the tools you need to cut through the fine print of your coverage. First, let’s review the types of insurance that are available on the market.
One of the most common types of insurance is private insurance offered through an employer. In this situation, your employer has negotiated a contract for you, the member, with a large insurance company like Blue Cross Blue Shield, Aetna, Cigna, and the like. Often, the employer will pay a portion of the monthly “premium” and the employee may contribute a portion for themselves or their dependent family members. A private insurance plan through an employer may be offered through a Health Maintenance Organization, or HMO, which gives members access to certain doctors and hospitals within its network, or a Preferred Provider Organization (PPO), which provides more flexibility when picking a doctor. Employers may offer several different plan options within the company. One employee may have different coverage than their office mate even though they both have insurance through the same employer and insurance company.
The second type of insurance is health insurance purchased on your own in the individual market. A great resource that outlines how to shop for individual insurance can be found here.
The article suggests first-time purchasers should strongly consider consulting several independent agents before buying a policy.
The third option for insurance coverage is a public insurance program like Medicaid or Medicare. Medicaid is the largest source of funding for medical and health-related services for people with low income in the US. Medicare is the federal health insurance program for people who are 65 years or older, and certain younger people with disabilities. You can find out more about qualifying for these programs by clicking here.
Stay tuned for more information on our insurance series, A Parent’s Guide to Navigating Insurance.
A Parent’s Guide to Navigating Insurance Coverage
JCCHD | Fri, May 15, 2015 | [Autism Treatment]Budgeting funds for your family’s healthcare costs can be a daunting task. How do you plan for up-front costs and make sure there are no surprise bills in the mail? Learning to understand your insurance coverage can be exhausting. We often hear people asking the same questions and sharing the same frustrations: Is my doctor in-network or out-of-network? How do I know how much I will get reimbursed for my appointment? I don’t understand my Explanation of Benefits, it might as well be written in Greek.
Checking in with your insurance company before an appointment occurs is a great way to arm yourself with information for allocating funds and preventing unexpected costs. But it is important to know what to ask and what to document when talking to your carrier or benefits coordinator.
Tune in to our free webinar A Parent’s Guide to Navigating Insurance Coverage on May 21st, and we will cover the frequently asked questions we hear from patients, parents, and caregivers. We will break down the types of insurance that are available on the market and what your coverage options are. We will define commonly used terms so you can speak knowledgeably to your clinician and understand your coverage. We’ll walk you through a sample bill and Explanation of Benefits so you’ll know what to look for when reading your own.
Have you had the dreaded experience of being denied coverage on an appointment or treatment? We will cover the process for appealing a denied claim. Are you embarking on a new treatment like ABA or speech therapy? Find out about the pre-authorization process and if it is required before you begin. Knowing your state’s insurance laws may help you get the coverage you deserve, and we’ll show you how.
We will also walk you through our step-by-step worksheet to complete when calling your insurance company about coverage. The worksheet will cover all the questions you need to ask your insurance representative to get the full picture on your coverage, and it will help you document conversations with insurance representatives to keep on file for future reference. At the end of the webinar, we’ll provide links to the downloadable worksheet and answer your questions.
Click here to register for this free webinar and take the first step toward tackling insurance coverage with confidence.
Teaching Kids Healthy Eating Habits
JCCHD | Thu, February 26, 2015 | [Family and Food][Healthcare]Children need the right fuel to grow, learn, and keep their energy levels up. With increased rates of childhood obesity, TV commercials advertising unhealthy snacks and food, and ongoing peer pressure, children might seem less inclined to make healthy choices. Although teaching healthy eating habits to your kids might seem like a daunting task, there are many things parents can do to engage their children in making smart food choices.

Monkey see, monkey do! Be a good role model.
Children are most likely to imitate their parents’ habits, and this can apply to food choices as well. Seeing you eat burgers and fries from the drive-through while they are being asked to eat fruits and vegetables can turn them off to the idea of eating healthy. Seeing you eat healthy will encourage your child to do the same. You can also teach your child about the importance of eating appropriate portions and ceasing to eat when you feel satisfied. Children should not feel as though they have to clean their plate, and having a conversation with them about portion control and fullness can lead to them making good choices for themselves when they sit down to eat. Taking a positive approach about food and eating right will encourage your children to do the same.
Get your kids involved.
Involving the children in meal planning or lunch-packing can encourage them to be more interested and invested in healthy eating. You can take them shopping with you and let them pick out their favorite fruits and vegetables or ones that they would like to try. Talk to the produce workers – they often have good suggestions, and may even let you sample new fruits and vegetables. For younger children, you can give them choices between two fruits or veggies and have them decide which one they would like to eat during a meal that week. You can help them categorize each item they pick out into each of the food groups to help them learn more about their food choices. You can also let your child plan a meal for the family to eat and encourage them to help prepare it. To make the preparation more fun, they can be “head chef” and plan out what items will be served in the meal. You can guide their decisions by encouraging them to include an item from food groups like fruits, vegetables, grains, and protein in the meal. When preparing the food, you can give them age-appropriate tasks so they can contribute. Kids can also get involved in packing their own lunches. When grocery shopping, have them pick out healthy snacks that they can they eat. Kids will feel in control of their decisions when choosing their own food options.
Make healthy snacks available.
If kids are around only healthy foods, they will certainly eat them! Keep your pantry stocked with healthy food choices. You can give your child options on healthy snacks, and they can choose which ones they would like to eat. Keeping a variety of foods is very important so children don’t get bored with the same options. This will allow them to explore new foods and flavors. Children need whole grains, fruits, vegetables, low-fat dairy (or another calcium source), and lean protein in order to grow and develop. Keeping a pantry and refrigerator stocked with items such as whole grain crackers, low-fat yogurt, and lean meat will ensure that your child will get the nutrients needed in order to grow and keep their energy levels up. Healthy eating is not limited to only food, however. Water is very important and encouraging your child to drink plenty of water throughout the day will help keep them from feeling fatigued and irritable. Try to avoid giving your child sugary juices and sodas, which are linked to increasing rates of childhood obesity and sap energy.
You can also have a conversation with your child about “go, slow, and whoa foods.” “Go” foods are those that are encouraged to be consumed on a regular basis, such as fruits, vegetables, skim milk (dairy or alternative), and whole grain crackers. “Slow” foods are those that can be consumed occasionally, such as peanut butter and baked potatoes. “Whoa” foods are the least healthy foods and should be consumed very rarely, if at all. Examples of “whoa” foods include french fries, fried chicken, and soda. Incorporating this system can help your children categorize their food options into healthy and unhealthy choices and encourage them to eat better.
Give your kids the freedom of choice.
Throughout this article, we have mentioned the importance of giving children choices. Children should feel in control of their decisions, and giving them options to choose from can help them feel this way. Being in control of their decisions can lead to confidence boosts in children, especially when these choices are positive. You can let your child pick between healthy snack options when packing their lunch or giving them an afternoon snack. Another thing that can allow children the freedom of choice is to incorporate family-style meals which allow them to choose what they would like to eat. The options on the table can also be healthy, of course, such as three different types of vegetables and two types of lean protein choices. However, children can make their own choice between these options. Another option is to include a base meal and several topping options. For example, for a taco, a base meal of tortillas and brown rice can be served, alongside toppings of lettuce, spinach, tomato, bell peppers, cheese, black beans, grilled chicken, and ground turkey. Children can decide which toppings they would like on their taco, but all options are healthy. This can also apply to pastas and salads.
Make food choices fun!
Not everything the child eats has to be healthy! Children can mix in small portions of their favorite treats in their meals. For example, you can include mashed chocolate chip cookies in their trail mix or add chocolate chips to a low-fat yogurt and fruit parfait. You can also make food choices fun by making their lunch or snack packaging appealing. Drawing doodles and cartoons on muffin tins or decorating their sandwich bags can make their food much more fun to eat. You can also add a note to their lunches. The note can be sweet sayings, a quote that can inspire them, a fun fact about a topic that interests them, or even a fact about the meal they are eating. The note can also compliment them on good food choices if they helped prepare the food. Making the meal more fun will encourage positive thoughts about eating well and making healthy food choices.
Assessment Corner: Identifying Autism After Brief Observations
JCCHD | Thu, February 26, 2015 | [Autism Treatment][Assessment Corner][Healthcare][News][Research]A recent article published by the journal Pediatrics, highlighted the challenges of accurately assessing children with autism spectrum disorders during brief observations. In primary care settings, medical professionals such as pediatricians and neurologists make critical decisions in screening and referring children who present with developmental delays and signs of autism. However, oftentimes the primary care setting only allows for very brief observations. This study analyzed what types of behavior and symptoms, both typical and atypical, can be optimally observed during ten-minute periods. It further investigated whether referrals for autism spectrum evaluations were made based on these observations.

The study included 42 children ages 15 to 33 months, some of whom were typically developing, and some who screened positive during an autism screening. Further diagnostic evaluations were completed to determine whether the children fit in the autism, language delay, or typical category. Licensed psychologists with expertise in the diagnostic evaluation of autism blindly reviewed two ten-minute video observations of each child and rated the following behaviors: responding, initiating, vocalizing, play, and response to name. Ratings of these behaviors as either “typical” or “atypical” were made. Raters were then asked whether an autism evaluation referral was needed based on the ten-minute observations.
Results showed that children with autism displayed more typical behavior than atypical behavior during the ten-minute observation periods. Furthermore, the psychologist raters made false negatives, and missed nearly 40% of the children in the autism group who would have needed an autism evaluation referral. This study emphasizes how difficult it is to make high-quality observations and form clinical impressions during brief observations of a child, common to primary care settings. It also makes the point that children with autism often display high rates of typical behavior alongside atypical behavior during short time periods, making it easy to miss red flags.
Findings illustrate that it is critical for primary care clinicians to utilize multiple sources of information when screening and making referrals for further autism evaluation, including behavioral observation as well as screening tools and parent report. Referrals for further assessment should be made when red flags are evident from all sources of information. Furthermore, best practice in the evaluation of autism spectrum disorders also includes the use of multiple sources of data such as comprehensive parent interview, parent questionnaires, and standardized measures (ex. the Autism Diagnostic Observation Schedule). Not only does a thorough evaluation provide a reliable and valid diagnosis, it also provides important information that can be used to identify skills and areas of need, and provide a benchmark for measuring change.
For the full text article see: http://pediatrics.aappublications.org/content/early/2015/01/07/peds.2014-1428
Gabrielsen, T. P., Garley, M., Speer, L., Villalobos, M., Baker, C. & Miller, J. (2015). Identifying autism in a brief observation. Pediatrics; 135 (2).
How to Safely Dispose of Medications
JCCHD | Wed, November 26, 2014 | [Healthcare][Q and A ]Unused and expired medications cause health hazards. Leaving medications in a cabinet makes them readily accessible to children and teenagers, creating a risk for accidental consumption and/or drug abuse. Flushing medication down the toilet contaminates drinking water; traces of numerous pharmaceuticals have already been found. This raises concerns for both human health and the environment. Therefore, proper management and disposal of medications is a necessary step in making children and the environment safer.
There are pharmacy and community drug-disposal programs that will accept medication and safely dispose of it. Dispose My Meds is a resource that can locate the participating pharmacy near you. There are also National Prescription Take Back Days ), which are enforced by the Drug Enforcement Administration (DEA). You may also contact the local trash and recycling service to see if such programs are available near you.

The last and least-preferred choice is proper household disposal. The drug label should provide instructions for safe disposal. If this is not the case, the FDA recommends taking out medication from the original container and mixing it in “an undesirable substance, such as used coffee grounds or kitty litter.” Put the mixture into a sealable bag and throw away. This can be done with tablets, capsules, liquids, gels, and cream, but not needles.
Needles should never be disposed of in the trash or recycling bin. This is dangerous to those around or near your trash, because they can be poked by the needles. There are drop off -disposal locations for needles too, just as with medications. Other options include special waste pickup services, needle-exchange programs, mail-back service, and home needle destruction devices. You can find more information about proper needle disposal at the Environmental Protection Agency (EPA) website and Safe Needle Disposal.
For more information on safe disposal of medications, please contact your local pharmacist or doctor. You can also find more information below:
Resources:
http://www.disposemymeds.org/index.php/environmental-impact
http://www.fda.gov/downloads/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/UnderstandingOver-the-CounterMedicines/ucm107163.pdf
http://www.safeneedledisposal.org/
http://www.epa.gov/wastes/nonhaz/industrial/medical/disposal.htm
Pets and Autism
JCCHD | Tue, November 25, 2014 |Pets play a big part in many children’s lives. Anecdotes have been circulating for years about the benefits of having a companion animal in the home of a child who has an Autism Spectrum Disorder (ASD) diagnosis. It is known that animals cause an increase in pro-social behaviors among typically developing children and adults. For example, people are more likely to engage in conversation with a person walking a dog than a person walking alone. Recently, more research has been done that provides evidence that interacting with animals is beneficial for children on the autism spectrum.
Research suggests that children with an ASD who interact with small animals (for example cats, dogs, guinea pigs, and rabbits) have significantly improved social behaviors compared to children with ASD who do not have the opportunity to interact with a small animal. Having a companion animal in the home beginning at age five improves two key social competencies: offering to share with others and offering to comfort someone.

A study published in 2013 showed that children with an ASD had enhanced social behaviors after playing with a guinea pig for ten minutes compared to when they interacted with toys for the same amount of time. These children engaged more often in talking, looked at faces, and made more tactile contact with people when an animal was present. Additionally, children with an ASD received more approaches and interaction from their typically developing peers when an animal was around, which can decrease social isolation.
Animals also increase the frequency of smiling and laughing in children with an ASD. And they can provide a source of unconditional love and support. In addition to increasing pro-social behaviors and being a comfort to children, recent research suggests the presence of an animal can decrease undesirable behaviors like aggression, grabbing, and social isolation.
Families with a child on the spectrum are often willing to try a variety of things to help their child. However, bringing a companion animal into your home is not a decision that should be made lightly. Animals require a lot of time, money, love, and attention, and may not be appropriate if these areas of your life are already stretched. Additionally, an allergy test should be performed on children who will be in the home with the animal to make sure there will not be any allergy issues. It is important to consider if the decision is appropriate for the whole family. It is important that a child shows interest in animals and that they can be trusted to interact with them safely. To determine this, have your child interact with a neighbor or friend’s companion animal first. If the child shows little interest, it may be best for you, the child, and the animal to consider alternatives to animal adoption. If the child is interested and responds positively, it may be something to consider.
References:
Carlisle GK. Pet Dog Ownership Decisions for Parents of Children With Autism Spectrum Disorder.
J Pediatr Nurs. 2014 Mar-Apr;29(2):114-23. doi: 10.1016/j.pedn.2013.09.005. Epub 2013 Oct 16.]]
Grandgeorge M, Tordjman S, Lazartigues A, Lemonnier E, Deleau M, et al. (2012) Does Pet Arrival Trigger Prosocial Behaviors in Individuals with Autism? PLoS ONE 7(8): e41739. doi:10.1371/journal.pone.0041739
O’Haire M. E., Mckenzie S. J., Beck A. M., Slaughter V. (2013). Social behaviors increase in children with autism in the presence of animals compared to toys. PLoS ONE 8:e5701010.1371/journal.pone.0057010
Kaminski, M., Pellino, T., & Wish, J. (2002). Play and pets: The physical and emotional impact of child-life and pet therapy on hospitalized children. Children’s Health Care, 31(4), 321-335.
Johnson, R. A., Odendaal, J. S., & Meadows, R. L. (2002). Animal-assisted interventions research: Issues and answers. Western Journal of Nursing Research, 24(4), 422-440
Solomon, O. (2010). What a dog can do: Children with autism and therapy dogs in social interaction. Journal of the Society for Psychological Anthropology, 38(1), 143-166.
Redefer, L. A., & Goodman, J. F. (1989). Brief report: Pet-facilitated therapy with autistic children. Journal of Autism and Developmental Disorders, 19(3), 461-467.
Martin, F., & Farnum, J. (2002). Animal-assisted therapy for children with pervasive developmental disorders. Western Journal of Nursing Research, 24(6), 657-670.
Wood, L., Giles-Corti, B., & Bulsara, M. (2005). The pet connection: Pets as a conduit for social capital? Social Science & Medicine (1982), 61(6), 1159-1173.
What Is A Social Skills Group?
JCCHD | Thu, November 20, 2014 | [Applied Behavior Analysis][Autism Treatment][Community][Q and A ]A social skills group is a valuable resource for building social skills for people with autism spectrum disorders. The group setting allows for participants to connect with peers and practice social skills, and provides the opportunity for modeling, role-play, and feedback. Groups usually include at least one facilitator, with three to ten group members of similar age and with similar goals. Sometimes typically developing peers are also involved in the group. Additionally, many programs include a parent group to help facilitate the generalization of skills learned to the home environment. Social skills groups can be geared towards any age group and level of social-skill functioning. For example, a group might consist of pre-school age children with emerging social skills, or
young adults who are higher functioning.
Are there certain curriculums or manuals that groups should follow?
Many groups follow a social skills curriculum or manual. One curriculum that has a strong evidence base is the PEERS program (Program for the Education and Enrichment of Relational Skills), which was developed at UCLA by Dr. Elizabeth Laugeson. The program is for adolescents and young adults with ASD. Groups are provided out of the UCLA peers clinic, as well as in other areas of the US. Manuals and books on how to apply the PEERS program can be found on their website, including a manual for teens, a manual for school-based professionals, and a book for parents and professionals called “The Science of Making Friends.” The UCLA PEERS clinic also offers training for group facilitators. Some examples of the types of skills that are targeted in the adolescent/teen group include: conversation skills, finding common interests, handling disagreements, and dealing with teasing.
An additional curriculum used for teaching social skills is the Social Thinking curriculum by Michelle Garcia Winner. Social Thinking is a concept that describes perspective-taking and how it impacts our social behavior and emotions. Several different workbooks that follow the Social Thinking methodology are available and can be integrated into social skills groups. Workshops and trainings are also available to professionals who want to utilize the principles of Social Thinking in their work.
Social Stories, created by Carol Gray, is an educational tool that can be integrated into a social skills group. Social Stories use a defined format to help model social scenarios that can help individuals with ASD identify important social information such as social cues and perspectives, and suggest responses.

How do I find a social skills group?
Social skills groups can be led by a variety of professionals; for example, Applied Behavior Analysts, Psychologists, and Speech and Language Pathologists. It is always helpful to get referrals from a reliable source, such as your child’s therapists. Parents might consider researching local autism-specific clinics, ABA clinics, or speech therapy offices to see if any offer social skills groups. Additionally, a simple internet search can display social skills groups in your area.
What makes a good social skills group?
The group should consist of similarly aged (both chronological and developmental) children with consistent social goals. It is always beneficial for parents to be involved to support generalization and the maintenance of skills learned. Applied Behavior Analysis is a highly evidenced intervention for individuals with ASD. Therefore, social skills groups that are facilitated by experienced ABA professionals are typically a reliable source for groups. Social skills groups should meet regularly, at least weekly, and for a sufficient amount of time, typically 12-16 weeks.
Krasney and colleagues (2003) reviewed existing literature on social skills groups and suggest the following guidelines for a well-run group:
- Teach concepts in a concrete manner
- Provide structure and predictability
- Simplify language and group children by level of language
- Provide numerous and diverse learning opportunities
- Include activities that require group work and cooperation
- Build self-awareness and self-esteem
- Set meaningful goals
- Teach goals successively
- Support generalization and maintenance of skills learned to relevant environments
What resources can help me learn more about social skills and social skills groups?
UCLA Peers Program: http://www.semel.ucla.edu/peers/teens
Social Thinking Curriculum by Michelle Garcia Winner: http://www.socialthinking.com
Social Stories by Carol Gray: http://www.thegraycenter.org; www.carolgraysocialstories.com
Autism Speaks: Social Skills and Autism http://www.autismspeaks.org/family-services/community-connections/social-skills-and-autism
Duke, M., Nowicki, S., Martin, E. & Holifield, V. (1996). Teaching Your Child the Language of Social Success. Atlanta, GA: Peachtree Publishing Ltd.
Taubman, M., Leaf, R. & Mceachin, J. (2011) Crafting connections: Contemporary Applied Behavior Analysis for enriching the social lives of persons with Autism Spectrum Disorder. New York: DRL Books
Smith, M. (2001). Teaching Play Skills to Children with Autism Spectrum Disorder. New York: DRL Books.
Krasny, L., Williams, B. J., Provencal, S., & Ozonoff, S. (2003). Social skills interventions for the autism spectrum: Essential ingredients and a model curriculum. Child and Adolescent Psychiatric Clinics of North America, 12(1), 107-122
Pumpkin: A Fall Favorite
JCCHD | Mon, November 17, 2014 |Ah, fall. It is the time of year when the air gets cooler, the leaves change color (at least in some places other than Austin), and our obsession with pumpkins reaches a new height. Pumpkin pie, pumpkin lattes, pumpkin soup, pumpkin pancakes, and pumpkin bread are just a few fall favorites. However, you may not know that pumpkins possess many health benefits.

Pumpkins are good for your vision.
Pumpkins are an excellent source of vitamin A, which aids in promoting good vision, particularly in low light, according to the National Institutes of Health. Pumpkin is full of the carotenoid beta-carotene, which converts to vitamin A and aids in maintaining vision health.
Pumpkins will keep you fuller longer, and they are good for your overall health.
One cup of cooked, mashed pumpkin contains about 2.7 grams of dietary fiber. Fiber helps keep you fuller longer, thus limiting frequent snacking and reducing the likelihood of consuming larger meal portions. This can help you achieve or maintain a healthy weight. Fiber is also good for your digestive system, as it reduces the risk of developing diverticular disease, which consists of hemorrhoids and small pouches in your colon. It also normalizes and helps maintain good bowel function.
Pumpkins are a good source of antioxidants.
Beta-carotene is also an antioxidant; and pumpkins are a good source of vitamin C, also an antioxidant. Antioxidants found from dietary sources such as pumpkins reverse the effects of free radicals in your body, which cause cell damage known as “oxidative stress,” and can reduce the risk of diseases like cancer, heart disease, Alzheimer’s disease, Parkinson’s disease, and even diabetes.
Pumpkins can help maintain normal body growth and function.
Pumpkins are a good source of potassium, containing about 12% of the recommended amount in one cup of cooked, mashed pumpkin. Potassium aids in several body functions, such as muscle growth, controlling acid-base balance, and maintaining the electrical activity in nerve and muscle cells in the heart.
Pumpkins can contribute to your overall well-being.
Pumpkin seeds are rich in tryptophan, an amino acid that is the building block for the neurotransmitter serotonin. High levels of serotonin can boost your mood and morale. It is also an important factor in regulating sleep and wakefulness—high levels of serotonin are associated with daytime, when one is generally fully awake.
Here are some recipes to try a fun, seasonal treat:
http://www.nourishingmeals.com/2011/10/grain-free-pumpkin-cupcakes.html
http://www.nourishingmeals.com/2008/11/giving-thanks-recipes-pumpkin-desserts.html
http://nomnompaleo.com/post/12318335046/paleo-pumpkin-coconut-maple-custard-cups
http://thevanityeffect.com/2013/02/nom-nom-paleo-pumpkin-cake/
http://deliciouslyorganic.net/grain-free-gluten-free-pumpkin-bread-recipe/
http://feedmephoebe.com/2013/10/the-balanced-diet-creamy-vegan-pumpkin-soup/
http://againstallgrain.com/2013/11/26/pumpkin-pancakes-bacon-pecans/
http://againstallgrain.com/2012/10/25/baked-pumpkin-doughnut/
http://againstallgrain.com/2012/10/09/pumpkin-spice-cookies-with-vanilla-cinnamon-icing/
Communicating with my Practitioner: Ways to Increase Successful Intervention in a Pediatric Setting
JCCHD | Fri, November 07, 2014 |Many people view a trip to the doctor’s office as a potentially stressful experience for the patient. While this may sometimes be true, it is important to recognize the potential stress for parents and caregivers. Parents may find the experience overwhelming, and, due to anxiety, they may forget to ask specific questions or fail to report significant information that could influence clinical recommendations. Below are some helpful tips that can aid both parents and practitioners in addressing these challenges and provide support to improve effective intervention.
Building a Rapport: Understanding the importance of the clinician-caregiver relationship is the first step. This is especially important in a pediatric setting where a parents’ report is the primary source of information. As a parent, it is essential to build a relationship with your team of clinicians in order to foster effective communication. From a clinicians’ perspective, this rapport is important in increasing successful intervention. Once trust is established, parents will feel supported and be more likely to implement recommendations. Rapport can also aid in future follow-up appointments. Parents may feel more confident scheduling follow-up appointments to discuss future recommendations or current concerns if they feel their practitioner is acknowledging their concerns.

Conveying Information: This is especially important for caregivers and parents to recognize. Even the smallest change or update can provide significant insight into how a patient is doing. Providing this information to your practitioner or clinical team is imperative. As practitioners, supporting honesty and open communication is the key to building accountability. Parents are more likely to report honestly if they do not feel ashamed or judged. Valuing that honesty can help bridge the gap in patient care.
Responsibility and Accountability: The more parents feel valued as active participants in the health care team, the more accountable they will feel in terms of implementing recommendations. If a rapport has been established, parents are more likely to discuss these changes with their practitioner as opposed to implementing treatment on their own. They may also feel a sense of responsibility toward their practitioner to implement recommendations or discuss any hesitations they may have.
It is important to address any questions and concerns to your health care team. Be honest, communicate effectively, build a rapport, and hold one another accountable in order to increase your chance of successful intervention.
Is Asperger’s Gone?
JCCHD | Fri, November 07, 2014 |Is Asperger’s gone? How have the changes made in the DSM-5 affected our children in schools and their ability to access care?
If you have a child with autism or work with families affected by autism, you have likely heard of “the DSM.” The DSM is the Diagnostic and Statistical Manual of Mental Disorders. It is published by the American Psychiatric Association and it is the primary manual used by clinicians to guide an autism spectrum disorder diagnosis. The latest edition, the fifth edition, was released in May, 2013.

One of the most significantly changed areas was the autism and developmental disorders section. The previous edition, the DSM-IV, included separate diagnoses associated with autism spectrum disorders: Autistic Disorder, Asperger’s Disorder, and Pervasive Developmental Disorder Not Otherwise Specified (or PDD-NOS). In the DSM-5, these separate diagnoses have been replaced with an umbrella diagnosis “Autism Spectrum Disorder” which is further defined by the level of severity of the individual’s deficits, with Level 1 being the least severe and Level 3 being the most severe.
This change has raised many questions and concerns. What happens to those previously diagnosed with Asperger’s Disorder? Many individuals with Asperger’s Disorder closely identify with the diagnosis and what it means for them. People have wondered, “does this mean I no longer have Asperger’s?” The DSM-5 notes that individuals with Asperger’s Disorder should not lose an autism spectrum diagnosis, stating “Individuals with a well-established DSM-IV diagnoses of autistic disorder, Asperger’s disorder, or pervasive developmental disorder not otherwise specified should be given the diagnosis of autism spectrum disorder.” However, if the individual is re-evaluated, the specific label will likely change. Despite this, clinicians have the flexibility to include the DSM-IV diagnosis of Asperger’s Disorder in their clinical reports, along with the new DSM-5 diagnosis. Therefore, there are definitely changes to the label, but Asperger’s Disorder will not disappear from an individual’s history.
Changes to the DSM-5 have also sparked concerns regarding how diagnostic changes will impact access to special education services. Schools use a separate system from the DSM for identifying individuals with autism, through the Individuals with Disabilities Improvement Act (IDEA), 2004 (300.8 (c) (1)(i); IDEA, 2004). If a child qualifies, an “educational qualification as a student with autism” is given based on the results of a Full Individual Evaluation (FIE) completed through the school district. Therefore, it is proposed that changes to the DSM-5 criteria should not directly influence services provided to students qualifying under educational law. Although, it is possible that changes to the DSM-5 will indirectly impact the educational system. For example, if a private evaluation is completed using the DSM-5, results might be reviewed and considered as part of a child’s FIE.
Overall, changes to the DSM-5 classification system are still relatively new and much is still unknown regarding the impact. Many private clinicians are just now transitioning to the use of the new criteria. It is critical that research is completed examining the use of the new criteria and its impact on individuals and services over time. It is also important that clinicians are knowledgeable about the changes and use their clinical judgment in applying the criteria. Ultimately, there is still much to be determined regarding the impact of the DSM-5.
A Smooth Trip from Takeoff to Landing
JCCHD | Fri, October 31, 2014 | [Autism Treatment][Community]Planning a vacation? Whether you are traveling by plane, cruise ship, or car, the key to smooth travel is in the planning.
Flying is often a brand new experience for children and may be more challenging for those with autism or developmental delays. Here are some steps to make travel as easy as possible.
Make a new experience as familiar as possible by making a picture book about your trip. Cut out photos of an airport, an airplane, and the flight crew. Paste in photos of the places or family members you will visit. Read this book in plenty of time to familiarize your child with the upcoming trip. Be sure to pack the book and have it ready for the ride to the airport.
Practice, practice, practice! A run-through of the trip preparations can help. Have your child help you pack some luggage and place it in the car trunk.
If you can do a run-through of the drive to the airport, or even take the shuttle bus, do so. You can also make the trip yourself and take photos along the way. Photograph the sea of cars in the parking lot, someone unpacking luggage from the car, and walking to the check-in area. If you are able to take your child with you, this is a chance to watch the airplanes land and take off and get acquainted with the new sounds of the airport. You can always record it on video to share at home.
Create a “Bon Voyage” bag. Pack your child’s favorite electronics, toys, games, headphones, music, and stuffed animals. Are there things you can buy in duplicate such that you can leave a set at home? It is easy to leave favorite items in the chaos of getting off a plane.
Don’t assume the airline food will be appropriate for your child. Add travel-worthy snacks to your Bon Voyage bag. As a precaution, ask your physician to write a doctor’s note to show to security in case your food items are questioned (this goes for on-flight supplements and medications as well). Will you be able to buy more of your special foods/snacks at your destination for your flight home, or do you need to pack extra in your checked luggage?
When dressing for the travel day remember that belts, jackets, and shoes may need to be removed at the security station. Slip-on shoes and zippers rather than buttons may be helpful wardrobe choices.
Have a visual schedule with activities for each 20 minutes of in-flight time, broken up by mini snack breaks. Even wrapping old items in gift wrap can add a “newness” to activities. The visual schedule will give your child something to look forward to the entire flight.
Warn your child that the airport may be noisy and crowded and review the airport photo and security photos. Remind your child that everyone takes off their shoes and coats at this point. Alert security that your child has special needs so they can expedite the metal detector screening. You may want to consider carrying a printed handout or brochure about autism and information about common behaviors that security personnel may not be familiar with.
Let the flight attendant know you would like to use the early boarding time to get your child settled before the airplane gets crowded.

Once you are on the plane, let a flight attendant know your child has special needs and notify him or her of any sensory sensitivities that may need to be accommodated (sensitivity to light and keeping the window shades down helps). Let the attendant know what has worked on past flights for your child.
Make the flight team aware that there may be an agitated response to a stressful situation on the flight, what it looks like for your child, and what measures you will take to help calm him or her.
It may help to choose a window seat to help keep your child seated. Walking up and down the aisles at regular intervals may be helpful.
As your plane comes in for a landing, review your photo book of exciting places and people you will visit upon arrival.
Have a nice trip!
Resources:
http://www.tsa.gov/traveler-information/autism-or-intellectual-disabilities
http://www.tsa.gov/traveler-information/travelers-disabilities-and-medical-conditions
http://www.phl.org/passengerinfo/Accessibility/Documents/SocialStories.pdf
http://www.tulsaairports.com/wp-content/uploads/2014/04/TUL-Social-Story.pdf
http://www.huffingtonpost.com/suzanne-robitaille/why-jetblue-started-an-au_b_3977300.html
Reducing Stress by Caring for a Houseplant
JCCHD | Fri, October 31, 2014 | [Community][Healthcare][Sibling Spotlight]We all know plants clean the air in our homes and offices, but did you know that they can also reduce your stress levels? There is something to that old cliché “stop and smell the roses.” It seems that everyone is too busy to step away from the daily grind and take a few minutes to be in the moment. This can be especially true if you are managing a schedule for an entire family. It is often difficult for a person to take time for him or herself. We tend to think of “me” time as selfish or unproductive, when it’s really imperative to reducing stress and maintaining peace of mind.
Caring for something with simple and defined needs, like a houseplant, allows us to step outside of ourselves and focus our energy on nurturing. The meditative acts of watering and trimming allow time for reflection. And knowing the plants are helping to clean the air and brighten up our environment makes it all the more rewarding.

The quiet routine of plant care is something you can choose to have all to yourself, or you can share it with your child. Here are some tips to make your nurturing time special:
- Learn all you can about your plant
Once you’ve chosen your plant, learn all of its maintenance needs, like appropriate amounts of water and sunlight. But also take the time to learn the history and origins. You may feel a special connection to a plant from a certain part of the world or one with a rich cultural history.
- Place it in a special spot
If possible, place the plant in a spot where you can see it often.
- Make caring for your plant a special routine
Instead of just throwing some tap water in a glass, take the time to use a special watering can, bring the water to an ideal temperature, and add appropriate plant food.
Taking a few quiet moments each day to care for a houseplant will give you a break from the external noise of life. Sharing that time with a loved one will make the experience all the more rewarding.
To choose a houseplant, check out this site. And to learn more about the care of houseplants, click here.
Oral Health and Autism Spectrum Disorders
JCCHD | Tue, October 28, 2014 | [Autism Treatment][Healthcare]Children with special needs like autism and Down’s syndrome generally have more cavities, gingivitis, periodontal disease, and missing teeth than the general population. This may be caused by a lack of oral hygiene and/or different medical and behavioral issues.
Eating too many sweets, not drinking enough water, grinding and clenching one’s teeth, pouching food rather than swallowing it, and taking medications that cause a dry mouth (i.e. antihistamines, anti-depressants, anti-psychotics, sedatives, and stimulants) are some of the reasons for the increased amount of cavities and dental issues in children with autism. This calls for regular dental visits and regular check ups. Don’t wait until your child is having a tooth emergency to see a dentist.
Medical issues such as a lack of hand coordination, strength, or agility make tooth brushing and flossing difficult, but not impossible with the right tools and attitude in place. Talk with your occupational therapist about ways to strengthen your child’s hand coordination. Some children have oral-sensory issues or anxiety about objects like a toothbrush in their mouth. You can play games and desensitize those fears. Talk with your local child life specialist or ABA therapist about desensitization methods, social stories, and other options.

Cavity and gum disease prevention are key in oral health. Start off by helping your child brush and floss their teeth on a daily basis. Get your child involved and excited by letting them help pick a toothbrush color or an appropriate location for brushing teeth. Set a schedule and start a route for your child so that they can learn to anticipate when it’s tooth brushing time. Use a visual schedule and/or a social story. Place visuals in the bathroom or tooth brushing location of the correct method of tooth brushing and flossing for your child to see and copy.
Going to the dentist can be a fun experience for your child. First, find a dentist who understands your child’s condition and specific needs, and one whom you trust and feel comfortable working with. Prepare your child for the visit by taking a field trip to the dentist’s office to get familiar with the facility and staff. Help your child practice sitting still like a statue in a dental chair and opening his or her mouth like an alligator several times. Read a social story and use visual sequence cards. Have a reward for the end of the dentist appointment. And perhaps most important, parents and caregivers should stay calm. Children perceive anxiety and will become anxious if they feel a need to be afraid. If you are calm, chances are your child will be calm too.
Useful resources:
https://www.upmchealthplan.com/pdf/HealthySmilesForAutism.pdf
http://www.autismspeaks.org/sites/default/files/documents/dentalguide.pdf
Don’t Let Allergies Bring You Down
JCCHD | Wed, October 08, 2014 | [Community][Healthcare]It’s that time of year again! Fall is that wonderful season when we get to think about sweaters, the upcoming holidays, and cooler weather. So heat up that cup of hot chocolate—but don’t forget about the tissues! While the weather change can often bring on seasonal allergies, there are plenty of natural remedies to help relieve allergy symptoms.

One popular trend is to use local honey to help address allergies, but the truth is that there is not enough scientific evidence to prove that it works. Continue to use honey as a natural sweetener, but don’t rely on it to relieve allergy symptoms. Here’s what you can consider doing instead:
1. Drink water. A person should drink about 8-10 cups of water per day. That may sound like a lot, but it will support your natural cleansing system, which can relieve allergy symptoms.
2. Drink green tea. Green tea has a powerful antioxidant that blocks histamine and immunoglobulin E, both of which can produce uncomfortable allergy symptoms.
3. Eat pineapples. Pineapples contain an enzyme that acts as an anti-inflammatory and blocks lung swelling.
4. Take a sip of apple cider vinegar. Yes, the smell and taste aren’t that appealing, but the health benefits are great. A teaspoon of apple cider vinegar a day makes the mucus production go away!
5. Add a bit of ginger to your water. Ginger is a good decongestant and antihistamine.
Embrace the cool weather coming in, but don’t forget that your health comes first.
It’s October – Time to Prepare for Halloween!
JCCHD | Mon, October 06, 2014 | [Community][Events][Sibling Spotlight]Halloween can be a very exciting, very stressful time of year for all families, including those with children who have special needs. Depending on the child’s age, challenges, and temperament, it can be difficult to predict if a child will enjoy, tolerate, or even be interested in Halloween. Here are a few tips for preparing your child.

Start talking about Halloween traditions and activities early on.
The easiest way to do this is by reading Halloween books or watching Halloween movies together. Use the stories to explain costumes, trick-or-treating, and common party games. You can even create your own social stories with pictures of your child, your family, and your neighborhood. If you decorate your home for Halloween, ask for your child’s advice and help. Be mindful of décor that may be too scary or not age-appropriate.
Get creative with costumes.
Some children with sensory issues may be reluctant to wear a costume. In that case, try one of these comfortable, familiar alternatives to a flashy costume:
Pajamas, robes, and/or slippers
A sports uniform, martial arts uniform, or dance-class attire
If your child does want a special costume, let them try on the costume at the store to make sure they are comfortable with it before buying it or try getting them involved in making a costume at home.
Trick-or-Treating.
Again, reading books, watching movies, and creating social stories are great ways to prep for Trick-or-Treating. You can practice trick-or-treating around the house, and take a walk around the neighborhood to familiarize your child with the area. You can plan your route and scope out different houses’ decorations and skip anything too scary or over-stimulating.
If door-to-door isn’t a good option for your child, check your community listings for trick-or-treating events in shopping centers, apartment complexes, or dormitories. Check if any local churches or community centers are hosting a trunk-or-treat event in their parking lot, or work with a group of parents and organize your own.
Keeping the sweets under control.
If your child has food allergies or intolerances, or you are concerned about sugar overload, check with local family dental offices to see if they are hosting a candy exchange. At these events, children turn in their Halloween haul for other prizes or raffle tickets. The collected candy is typically donated to a local food pantry, domestic violence shelter, or sent overseas to soldiers in care packages. If you can’t find a candy exchange near you, come up with your own candy trade-in system based on your child’s interests. For example, 25 pieces of candy can equal a trip to the movies, or 10 pieces of candy for a new book. Some parents get creative and set up their own little store!
Preparing your child for Halloween traditions and having a plan in place for events are the keys to minimizing the stress and making the most of the holiday. At The Johnson Center for Child Health and Development, we host an annual Halloween party to provide a fun, safe way for families to enjoy Halloween traditions. The party is held before Halloween, so the kids can practice wearing their costumes and trick-or-treating. As with all of our events, we provide allergen-friendly snacks, crafts, a photo booth, and other special surprises. This year, the party will be held on Thursday, October 30 from 3:30pm-5:30pm. The party is free and open to the public, but we do ask that you RSVP so we have enough treats for all (email .(JavaScript must be enabled to view this email address) to RSVP). Kids of all ages are welcome and costumes for everyone are encouraged, but not required. We will all certainly be in costume and hope to see you there!
Protect Yourself While Eating Out
JCCHD | Wed, October 01, 2014 | [Family and Food][Healthcare]Have you ever had food poisoning? If so, you would probably do anything to avoid getting it again. Here are some tips on safely navigating eating out at restaurants:
Does your food look funny? Smell funny? It should smell appetizing and make you want to dive in. If it smells questionable, don’t doubt yourself…send it back.
Don’t order fish at the beginning of the week. Often Saturday night fish specials will be kept until Monday if they don’t sell out.
Be your own inspector. Take a close look at your meat or poultry to make sure it is as thoroughly cooked as you would like it to be.
Ask the waiter what the most popular dishes are. More popular items have less chance of hanging out in the restaurant refrigerator. Specials may be “dressed up” items that didn’t sell as expected.
Know your A, B, C’s. Many health departments post a restaurant grade at the restaurant or check the health department website for a restaurant grade before you make the trek out.
If you question your restaurant at all, visit the restroom and see if it is well cared for. If not, peek in the kitchen if you can—if you spot cleanliness issues, you may rethink your choice and leave before you place your order.
A loud, busy restaurant is a good sign. If your choice is void of customers, the wait staff is standing around, and you notice the neighboring restaurants are bustling with guests, it may be a sign to move on.
Ah, the buffet. So many choices of bacteria growing on the lukewarm setting. Is it worth the risk? While it doesn’t need heating, the salad bar is its own buffet of bacteria and is often a good idea to pass up. Avoid the buckets of salad dressings and sauces and ask if they have individual packets for take-out. These rules also apply to the neighborhood pot luck or picnic where food is not kept at appropriate temperatures.
Stuffed? Take the leftovers in a doggy bag, but be sure to refrigerate it within two hours. If the car is hot [90 degrees or more] get it in the fridge within one hour. If you forgot that delicious meal and find the leftovers the next day—well, best not to take the gamble. If it looks odd or smells funny, toss it.
If you do get food poisoning, alert your dining companions. They will appreciate the heads-up. If you feel like you can pinpoint the contaminated food source, be sure to call the store or restaurant and let them know.
A little extra caution can go a long way. So stay alert and bon appétit!
Focus on Routines…But Don’t Overschedule
JCCHD | Tue, September 02, 2014 | [Healthcare][Sibling Spotlight]Routines are great, but over-scheduling can cause stress for the whole family.
In a recent post, we highlighted the importance of routine in a child’s life. The benefits of a routine for children and teens are numerous and well-documented. But it can get dicey when a well-meaning parent rigidly schedules every minute of a child’s day.
With increasingly intense academic demands and daunting schedules imposed on kids today, it’s easy for parents to get caught up in extra-curricular activities, sports, tutoring, music lessons, et cetera. And when a child has special needs, many of those activities are scheduled along with therapies and appointments. We want to give our children every chance we can to be productive and competitive, and we can forget the best reason to expose them to different activities: to provide them the opportunity to find their own way.
Down time is very important to a child’s journey of self-discovery. Boredom can be a powerful thing. In those moments, kids listen to their inner voice and discover what really makes them happy. Over-scheduling does not allow time for self-reflection.

While it is beneficial to let your child try new things, and even to gently push them to do an activity or learn a skill they may not immediately like, it’s important to listen to them and pay attention to their interests.
You can help by making sure that your child has adequate homework and study time. Be actively informed of their workload and block off an appropriate amount of time. Cutting into study time can often lead to cutting into sleep time.
Also keep in mind that sit-down dinners are very beneficial to your family’s overall health. When you take the time to plan a meal and eat together, you are much more likely to make good nutritional choices that will help fuel the rest of your day.
While planning your child’s routine, here are some suggestions of which “times” should stay consistent, and where to leave room for flexibility and creativity:
Keep a consistent routine with:
-Wake-up time
-Meal times, including a sit-down
-Homework time
-Bed time
-Prescribed therapies (speech, occupational therapy, physical therapy, etc.)
Fill in the blanks with a balance of:
-Organized activity/lesson time
-Friend/social time
-Family time
-Down time
And remember, when you manage your own time well, it serves as a great example for your entire family.
Resources:
http://www.education.com/magazine/article/Benefits_Underscheduling_Child/
http://www.healthychildren.org/English/healthy-living/emotional-wellness/Pages/Avoid-Over-Scheduling.aspx
http://www.webmd.com/parenting/guide/parenting-mistakes-with-grade-school-age-kids
http://stress.about.com/od/studentstress/a/school_anxiety_2.htm
Gluten Free Labels and How They Affect Us
JCCHD | Tue, September 02, 2014 | [Family and Food][Healthcare][News]Fad diets influence food manufactures to market to those seeking healthy alternatives to mainstream snacks and treats. While roaming through the grocery store, some consumers might mistakenly believe that products with labels advertising gluten-free ingredients are healthier choices. The desire to investigate the nutritional content is replaced by the confidence of knowing that it’s gluten-free. The label itself influences the choice we make for our family. Now, thanks to the new standardized definition from the FDA, we can move forward with additional awareness on what that label actually means.

The new FDA regulation of August 2014 requires that products labeled as gluten-free contain no more than a maximum of 20 parts per million of gluten. This has typically been the standard for quality producers familiar with gluten and its impact on health, but it has not been a requirement until now. What does this mean for the general population, particularly those suffering from a gluten intolerance or Celiac disease? Gluten-free products will now have to adhere to a stricter standard. While this does address the issue of mislabeling foods, it does not in any way define the nutritional value of these products.
The term “gluten-free” does not automatically mean that any food is healthy for you—many gluten-free products are no more than junk food. Determining the health benefits of any item requires knowledge of various factors, including your own individual health status and specific dietary needs. To become truly educated and informed, talk to your local dietician or nutritionist regarding your specific health concerns. Understanding the label is the first step. Educating ourselves on how the food itself affects our bodies is the next.
What Labor Day Means To Us
JCCHD | Mon, September 01, 2014 | [Community][News]Labor Day is the celebration of the American labor movement and it is dedicated to the social and economic achievements of workers. According to the US Department of Labor, “it constitutes a yearly national tribute to the contributions workers have made to the strength, prosperity, and well-being of our country.”

This year, as we reflect on the holiday and its meaning, we can’t help but think about the thousands of adolescents and adults who are eager to make such a contribution, but are prevented from doing so because of the lack of opportunities and misperceptions about their abilities. In June of 2012, the US Bureau of Labor Statistics reported that just 32.1% of Americans who have a disability are employed as part of the nation’s workforce. Autism Speaks subsequently reported that 9 out of 10 adults with autism were either unemployed or underemployed, regardless of their IQ or education.
There are several studies published that discuss these statistics and the issues of unemployment, underemployment, pay discrepancies, and the hardships that these issues present to adults with autism. The bottom line is that there are far too many people with autism who are capable of employment who are not given the opportunity to work. This leads to depression, isolation, and financial hardship. What’s more, our country is deprived of the contributions that these potential workers can make. People with autism have a lot to offer, and by failing to offer support, training, and opportunity, we are missing out.
The Johnson Center employs people with autism in our office. We have had young students with autism who are in high school and college complete internships in our office as they prepare to graduate. This issue is personal for many of us, who have teenage and young adult children of our own who have autism. We have seen first hand the challenges these remarkable young people face when seeking employment and the gifts they can bring to the workplace when given the chance.

Sometimes the issue is ability and support. There are an increasing number of colleges that offer programs and support for young people with autism. There are a growing number of high school and college programs that are taking innovative steps to prepare their students for the workforce. There are vocational rehabilitation counselors who can provide assistance in finding and training for the right job. And there are some families who take matters into their own hands and start their own businesses.
Sometimes the issue is opportunity. Most employers don’t know the facts when it comes to employing a person who has autism. They don’t know that there are many jobs that people with autism may be uniquely qualified to do and they are unaware of the benefits such a hire may provide them.
We experienced this lack of knowledge recently when we reached out to a local pet store chain that had announced they were hiring. We know a young man with autism who is very interested in and skillful with animals. He is a hard and dependable worker and we hoped to match his skills with his interest and help him find a job he would enjoy and excel at doing. We called all six of the locations of the chain and were summarily dismissed as soon as we explained what we were trying to do. One store manager even hung up on us as we explained why we were calling.
So we are taking this Labor Day as a call to action: learn the facts about autism and employment and encourage your employer, businesses you frequent, and friends and family to consider employing people with autism. Connect them with resources and vocational training centers that can offer support. We all have a vested interest in opening doors for people with autism; it will help our loved ones and help our communities. And it will allow thousands of people with autism to contribute to the “the strength, prosperity, and well-being of our country.”
Resources:
In addition to the links in the article above, here are some resources to learn more on the issue…
http://www.dps.missouri.edu/Autism/AutismFactSheet2011.pdf
http://www.dol.gov/odep/
http://www.disabilityscoop.com/2013/08/05/with-training-jobs/18446/
http://www.npr.org/blogs/health/2013/04/22/177452578/young-adults-with-autism-can-thrive-in-high-tech-jobs
http://www.grandin.com/inc/transition.employment.autism.aspergers.html
http://www.huffingtonpost.com/2012/09/27/autism-employment-white-collar-jobs_n_1916611.html
Refresh Your Sleep Schedule for Back-to-School
JCCHD | Tue, August 26, 2014 | [Healthcare]Back to school time is here and after a summer of staying up late and sleeping in, children can have a hard time adjusting to school’s early start time. Not only is it not much fun to be tired during the day, it can also affect academic performance. Studies show that too little sleep can cause an inability to concentrate, dozing off in class, behavioral issues, and lower level social skills. Persistent sleeping problems are associated with learning difficulties. One study demonstrated that as little as 25 minutes of less sleep a night can cause poorer grades. Students who received “C” and “D” marks went to bed on average 40 minutes later than “A” and “B” students. The good news is there are a few, easy steps parents and kids can take to ensure a better night’s sleep.
It is a good idea to begin adjusting your child’s sleep habits about two weeks before school starts. Going to bed 15 minutes earlier each day until the desired bedtime is reached is recommended. This allows children to adjust gradually and ensure a smooth transition to better sleep habits. Make sure nighttime routines are consistent. For example, you may want to have your child get into their PJ’s, brush their teeth, and then read a story before bed every night. This allows the child to associate a pattern of activities with sleepiness. A child’s room should be cool, quiet and comfortable. It should also be free of distractions, especially screens, like TVs, computers, phones, and video games.
During the day you want to make sure your child limits the amount of non-sleep activities he or she does in their bed. For example, it’s better for a child to study or read at a desk or couch than in their bed because then the bed becomes associated with wakefulness rather than sleep. You also want to make sure to limit the amount of caffeine (tea, chocolate, and soda) your child has, especially in the afternoon and evening. Caffeine can cause children to have trouble falling asleep and can lead to more restless sleep. Lastly, eating a healthy diet and exercising daily can help your child have a good night’s sleep.
By following these tips your child will be able to refresh their sleeping habits and start the school year off right!
Can you help?
JCCHD | Thu, August 21, 2014 | [Community]In the ten years since we started our work, we have had the privilege of working with amazing children and phenomenal families. Often we have been with them as they have faced significant health issues, traumatic family crises, and severe emotional strain. We try to serve them to the best of our ability, but every so often we need to ask for the help of our community. This is one of those times.
We have worked for the last eight years with a family who lives in a small town near College Station, TX. Cindy is a single mother who has been diligent and productive in seeking support and care for her four children, including her now 14-year-old son with autism and a daughter with Cystic Fibrosis (she also has a son in college and an 11-year-old son).
Tragically, Cindy’s daughter passed away three years ago; since then they have worked hard to address the emotional and financial hardships that have come their way. And now they face another tragedy: lightning struck their home on Tuesday and it caught on fire. One of the boys was home and managed to escape with the family dogs, but other pets perished in the fire and the home is destroyed. The family lost everything, including priceless mementos of their daughter.
While we can’t replace those precious items, we do want to help this family turn the tide on a tragic chain of events and help them rebuild and start what will hopefully be a happier phase of their lives. And this is where we hope our community can help.
We are collecting items to help this family get back on their feet. If you can help with any items from the following list, please let us know. Our staff will also be contributing and we will be driving out to see the family in nine days to take them the gifts we have collected.
One of the hallmarks of our community has always been empathy, spirit, and generosity. We thank you in advance for what we know will be an outpouring of love and kindness to lift this family up in their time of need.
Wish list:
The family currently does not have a place to live, so the most pressing needs are portable ones: clothing, toiletries, and games for the kids.
Once they have a place to live, they will need all of their household goods replaced.
Their car is also now out of commission, so transportation is an issue.
If ANYONE knows of a house or apartment in the Normangee area that may be available please let us know.
If anyone has the use of a reliable car that seats at least four that the family could use, or knows a mechanic in the area who can help repair their car, please let us know.
Current pressing needs:
- Clothing:
Long pants: size 12 slim and 30/30
Jackets: size 12-14 boys and 18 Boys or Adult Small
Shoes and flip-flops: size 8 (preferably with Velcro) and size 6.5-7
- Shopping bags, suit cases
- Toiletries: Hair brushes, combs, toothbrushes, lotion, soap
- Towels, blankets, pillows
- Gift cards: HEB, Wal-Mart, Whole Foods, Amazon, Walgreens, CVS,
- School supplies, reusable lunch bags/boxes, Stainless Steel Water Bottles, Backpacks
- Electronics: Nintendo DS, video games (Godzilla, Shreck, Scooby Doo), computer/lap top
Once they have a semi-permanent location, they will need housewares: pots, pans, plates, and utensils. They will also need basic furniture (beds, lamps, tables and chairs).
Please contact us at .(JavaScript must be enabled to view this email address) or 512.732.8400 if you would like to help.
Update: Gift cards, clothing, toiletries, games, and notes of support can be delivered to our office and we will deliver to the family.
The Johnson Center for Child Health & Development
Attention: Family Support
1700 Rio Grande, Suite 200
Austin, TX 78701
Shop for Safer School Supplies
JCCHD | Wed, August 20, 2014 | [Community][Healthcare]Any parent of a school-aged child knows how many choices there are for back-to-school supplies. Before deciding which comic book hero or cartoon cat your child wants on his or her binder, check labels and choose one that isn’t risky for their health or the environment.
Commonly used materials like PVC/vinyl contain high levels of phthalates, an additive used to soften plastics. Phthalates can leech out of products over time, contaminating food, being absorbed through skin, and even evaporating into the air we breathe. Exposure to phthalates has been linked to asthma, learning disabilities, diabetes, and other chronic conditions. Children are at a high risk from long-term exposure to phthalates and other chemical additives because their bodies and brains are still developing. This risk has been addressed somewhat in the US by banning phthalates from children’s toys, but dangerous levels are often still found in school supplies.
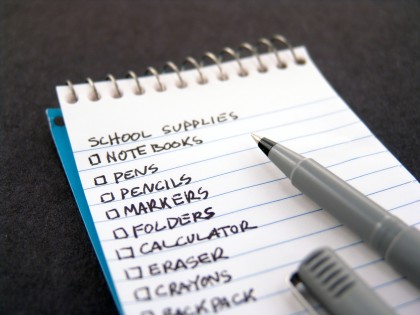
The manufacture, use, and disposal of phthalates also pose a huge environmental risk. The heat generated in manufacturing or burning phthalates releases highly toxic chemicals known as dioxins into the air, the ground, and the water supply. These dioxins are known to cause harm to immune and reproductive systems, as well as causing cancer.
You can determine which school supplies to avoid by reading labels. Usually a product made out of vinyl or PVC will say so on the label. If not, check the recycling symbol. If the symbol contains the number 3, the product is made out of PVC. If you cannot find the symbol, be a pro-active consumer. Research the manufacturer’s web site or call the customer service number.
Doing your homework to keep your own family safe is great, but consider taking it a step further. Organize with other parents and teachers to start a green initiative in your child’s classroom, school, or district.
Check out these resources for toxin-free and sustainable school supplies:
http://greenschools.net/article.php?id=177
http://www.chej.org/publications/PVCGuide/PVCfree.pdf
http://www.theultimategreenstore.com/s-59-eco-school-supplies.aspx
Be An Early Riser
JCCHD | Sun, August 17, 2014 | [Healthcare]From peer-reviewed journals to trendy buzzword articles, the advice to “be an early riser” is all around us. Articles, columns, and blog posts from all corners of the media tout the benefits of waking up early. They tell us that early birds, or “larks,” are happier, more proactive, have more free time, and are more organized. But how exactly does that translate to a healthier life?
Research shows that getting an early start to the day is the first step in making healthy choices all day long. The extra time afforded by rising early allows busy parents to exercise or prepare healthy breakfast and lunches. Professionals who get to work early enjoy an easier commute and some uninterrupted time at the office. This allows them to leave on time or bring less work home so they can spend time in the evening relaxing.

Surveys have shown that early risers are better organized, using the time to set goals and plan out the day or week ahead. This can translate to healthy meal planning, making time for exercise, or planning fun family activities.
On a biological note, studies suggest that people who go to bed and rise early are more in tune with the body’s natural sleep cycles triggered by the daylight cycles. This could be the reason why early risers report better overall sleep quality.
Ultimately, the health benefits of rising early are twofold: both physical and mental. Better sleep and more time for exercise and meal planning make for a healthy body, while organization, reduced stress, and relaxing personal time clears the mind.
References:
http://www.forbes.com/pictures/ehjh45khem/benefits-of-early-risers-2/
http://www.telegraph.co.uk/health/healthnews/9327244/Why-the-early-bird-is-happier-and-healthier-in-life.html
Prioritize Healthy School Lunches
JCCHD | Sun, August 17, 2014 | [Family and Food][Healthcare]Whether you buy a hot lunch for your child or pack a bento box, brown bag, or vintage metal Batman lunchbox, prioritizing a healthy lunch is critical. Eating a variety of healthy foods can give your child energy, improve their learning, and build healthy habits.
As you write out the to-do lists for back-to-school, make a plan to ensure your child will eat a healthy meal at school each day.
If you plan to buy hot lunches through your school, give the menu a close look and know what options might exist. Is there a salad or sandwich bar available? Are there ways to avoid less healthy choices that are full of sugar? Review the menu with your child and talk about the options, encouraging him or her to give the healthy foods a try. If you can, join your child in the cafeteria and talk about the menu options and how to make good choices.
If your child has food allergies, talk to the school and partner with the food services staff to come up with appropriate menu options. Make sure they know who your child is and are up-to-date about what alternatives may be available. Educate your child and teach them to speak up and ask questions about what they are eating. We know 4-year-olds who are not shy about speaking up about their allergies!

If you choose to pack a lunch, add the appropriate supplies to your back-to-school shopping list. Bento boxes, Laptop Lunchboxes, and similar supplies all make packing up a healthy lunch quite easy. Be sure your containers are BPA-free and easily cleaned. Get in the habit of making the plan in advance, either over the weekend or the night before, to avoid the last minute rush.
Include your child in the meal planning and preparation. If a child is involved in choosing their lunch, they are far more likely to eat it. There are several age-appropriate tools to help facilitate this process, or you can make your own. Check out this chart as an example. There are many creative ways to make lunches from home more fun. Use cookie cutters to cut fun-shaped sandwiches, cut your fruits and vegetables into shapes, and throw in an encouraging note or love card.
There are many great resources online to help you avoid or break out of a lunch rut. Talk with your family about their preferences and learn what students around the world eat for lunch. Most importantly, have fun with it and use it as an opportunity to teach your child skills and lessons that will serve them for a lifetime.

Know the Ebola Facts
JCCHD | Wed, August 13, 2014 | [Healthcare][News]Ebola is a disease caused by a tropical virus. It causes flu-like symptoms: fever, headache, joint and muscle aches, general weakness, diarrhea, vomiting, stomach pain, and loss of appetite. As the disease progresses, the body experiences organ failure, dehydration, and bleeding. The current outbreak is concentrated in West Africa.
Ebola cannot be transmitted through the air, food, or water. It is not like the flu, which can be passed on through coughing and shaking hands. People become infected with Ebola when they come into contact with an infected person’s sweat, blood, vomit, or feces. This usually happens when family or medical workers treating a person infected with the virus come into close contact with these substances without wearing the right medical equipment (gloves, goggles, and masks), or because they use unclean medical instruments (needles and syringes). If proper precautions are taken, the transmission of the virus can be controlled quickly.
Health organizations are not overly concerned about the disease coming to the United States. Healthcare and airport screeners understand the disease and know how to prevent its spread. They can look for symptoms in people coming from an affected area and make sure they are healthy enough to enter the US. The US also has a high level of health care and can help treat anyone who is sick by providing appropriate isolation, necessary fluids, and monitoring health stats. Doctors in the US also use safety equipment and clean medical supplies to prevent the spread of disease. All of this reduces the likelihood that Ebola will be a health issue in the US.
The best lesson we can take from the news of this outbreak is that it is always a good idea to practice good hygiene and use good common sense, especially when traveling. Washing your hands frequently, avoiding people who are sick, and keeping people who have a fever home and away from others are all great examples of ways we can help to stop the spread of many diseases, from colds and the flu to more serious ones like Ebola.
Daily Routines for a Happy, Healthy, and Successful School Year
JCCHD | Wed, August 13, 2014 | [Community][Healthcare][Sibling Spotlight]It’s everybody’s favorite time of year—back to school! Okay, maybe not everyone’s, but there are a few important ways parents can help their kids thrive in this changing environment. With the new school year comes many changes in our children’s lives. These changes can often be scary and overwhelming, causing our child’s performance to suffer in many different areas. There is nothing that can alleviate these types of stressors for our kiddos like well established routines.
Although many adults find routines mundane, it is well known that kids flourish when there is more structure in their lives. “Knowing what to expect from relationships and activities helps children become more confident,” says Dr. Peter Gorski, assistant professor of pediatrics at Harvard Medical School in Cambridge, Massachusetts (Liza Asher, 2009). It is important for kids to have routines at home because it gives them a sense of security that can help with the stress of starting a new school year. Effective routines at home can also help to develop the self-discipline that will help them later in life. Just like the rest of us, children handle change best if it is expected and occurs within a familiar routine. A predictable routine allows children to feel safe, and to develop a sense of mastery in handling their lives.

Establishing effective routines that strike a good balance between the chaos of unstructured time and overbearing rigidity can be challenging (American Academy of Pediatrics, 2004). It is important to stay consistent when following through on everyday routines, but it is equally important to leave some room for flexibility. Learning how to navigate structure and routines with flexibility teaches kids how to constructively control themselves and their environments.
Most parents already know that their children learn a great deal from them—even bad habits are easily learned through simple observation. This is why it’s important to practice what you preach and show your children examples of good planning and organizational skills in your own life. Two of the most important routines for children involve following regular meal times and learning how to wind down before bedtime. These routines should be practiced by everyone in the family, if possible, for the benefit of all.
There is a long list of benefits for children as well as the whole family when effective routines are followed. Routines can eliminate power struggles when activities like teeth brushing or turning off the TV are just the things that are done at a certain time of the day. Children following a routine will be better prepared for transitions and will therefore have lower stress levels. When children are proficient at their daily routine it gives them a sense of accomplishment and independence that will make them less likely to become oppositional. And getting on a schedule helps kids and adults fall asleep sooner, making them both physically and emotionally healthier.
These are just a few of the benefits—it’s hard enough to start a new school year with new teachers and new friends. These tips can help set up your child for an easy transition into a happy, healthy, and successful school year.
References:
American Academy of Pediatrics. (2004). Why are family routines so important to children?. Healthychildren.org, retrieved from http://www.healthychildren.org/English/family-life/family-dynamics/Pages/The-Importance-of-Family-Routines.aspx
Asher, L. (2009). The Importance of Routines for Children. Mommd, retrieved from http://www.mommd.com/routines.shtml